An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Scoping review of obesity interventions: Research frontiers and publication status
Longhao zhang, tingting jin.
- Author information
- Article notes
- Copyright and License information
Corresponding author [email protected]
Corresponding author [email protected]
These authors contributed equally
Collection date 2024 Apr 19.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Obesity and overweight are significant global health issues, and numerous obesity intervention studies have been conducted. Summarizing current knowledge of interventions aims to inform researchers and policymakers to keep up-to-date with the latest scientific advancements and trends. In this review, we comprehensively retrieved and screened 4,541 studies on obesity intervention published between 2018 and 2022 in the Web of Science Core Collection, and objectively presented research frontiers using bibliometric analysis. The research frontiers of intervention are mainly focused on dietary, exercise, pharmacological interventions, bariatric surgery, environmental, and cognitive interventions. Time-restricted eating is the hottest research topic, followed by probiotics and Roux-en-Y gastric bypass. Gut microbiota is located in the “Basic and transversal themes” quadrant with a high centrality and low density, which has great development potentiality. Obesity intervention is becoming increasingly common,and we advocate for researchers to undertake more focused research endeavors that consider the specific characteristics of diverse populations or patients.
Subject areas: Medical science, Clinical finding
Graphical abstract
Medical science; Clinical finding
Introduction
With the acceleration of industrialization and urbanization worldwide, obesity has become the highest incidence of chronic diseases, affecting approximately 650 million individuals. 1 Obesity and overweight are global health problems and have been associated with a variety of diseases such as diabetes, cardiovascular diseases, tumors, skeletal diseases, and digestive system diseases. 2 Scientists have increasingly understood that obesity is a complex multifactorial metabolic disease that involves central and peripheral energy balance regulation, and helping some obese individuals recover and maintain weight through lifestyle regulation alone may prove difficult. 2 , 3 , 4 In recent years, there has been a surge in obesity intervention studies worldwide, with new and diverse measures emerging to improve weight loss and combat obesity. Relevant researchers and stakeholders are required to grasp the scientific research progress and hot spot trends in the fields. However, to date, in the face of the multitude of complex research information, a systematic and objective review of obesity intervention is lacking to assist with understanding the complexity and hotspots of research topics and to extract accurate and valuable information effectively.
The bibliometric and visual analysis can objectively provide a unique perspective to show an overall view of the current status of the research on obesity intervention and reveal the context of scientific research. 5 Research frontiers can also be identified through analysis of the cited patterns and clusters of articles on specific topics, especially the frequent co-citation of clustered highly cited articles. 6 This has become particularly important with the development and rise of evidence-based practice. In addition to mapping the research status, bibliometrics can also determine the topic “hotspots,” that is, the topic clusters of related topics, which can be displayed by knowledge maps or inductive lists, which will provide guidance for clinical practitioners and researchers. In this study, we utilized the aforementioned analytical method to more fully demonstrate and explore the developmental context of research to obesity intervention. Specifically, our aim was to summarize popular interventions aimed at improving obesity and weight loss, present the research frontiers in this field, analyze the contributions of different nations, institutions, authors, and journals, as well as conclude on the most cutting-edge interventions to improve obesity and overweight. This study is expected to help researchers gain a better understanding of the current research status of obesity intervention and identify new directions for future research.
A total of 4,541 English-language articles were retrieved and screened from the Web of Science Core Collection. The h-index is a metric used to measure the impact or influence of a researcher’s publications, based on Web of Science citation data. Self-citation is defined as citations that refer to a work by one of its authors. They, in the Web of Science databases, play important roles in evaluating the productivity, impact, and influence of researchers’ work. The total h-index of the 4,541 publications was 63, the average number of citations was 9.32, and the total number of citations was 42,314 (without self-citations 39,214). From 2018 to 2022, the number of publications generally increased, with the highest number in 2021 (1,042), but slightly decreased in 2022 (874). These articles were published in 1,128 journals, of which the most published journals were Nutrients (292, 6.43%), International Journal Of Environmental Research And Public Health (111, 2.44%), and Bmc Public Health (104, 2.29%).
Mapping publication status
Country/region distribution and cooperation network.
A total of 99 countries and regions were involved in publishing these 4,541 articles. Specifically, the top 10 countries that published most articles were the United States (1,756, 38.67%), Australia (443, 9.76%), the United Kingdom (429, 9.45%), China (305, 6.72%), Spain (270, 5.95%), Canada (235, 5.18%), Brazil (233, 5.13%), Germany (230, 5.07%), Iran (207, 4.56%), and the Netherlands (193, 4.25%), in which only China and Brazil are developing countries. There is a greater number of developed countries that are actively involved in and conducting research in related fields, while the number of developing countries is comparatively smaller. Evidently, the contribution of developing countries in obesity intervention research publications lagged behind that of developed countries.
From the perspective of the national cooperation network, the countries involved in the included literature were primarily divided into four groups according to their internal connections, among which the two groups led by the United States of America and England occupied a major position in the entire network, as shown in Figure 1 . The number and thickness of the connections reflect the frequent and close cooperation between groups led by the United States of America and England, including Germany, Spain, Australia, Canada, and Denmark.
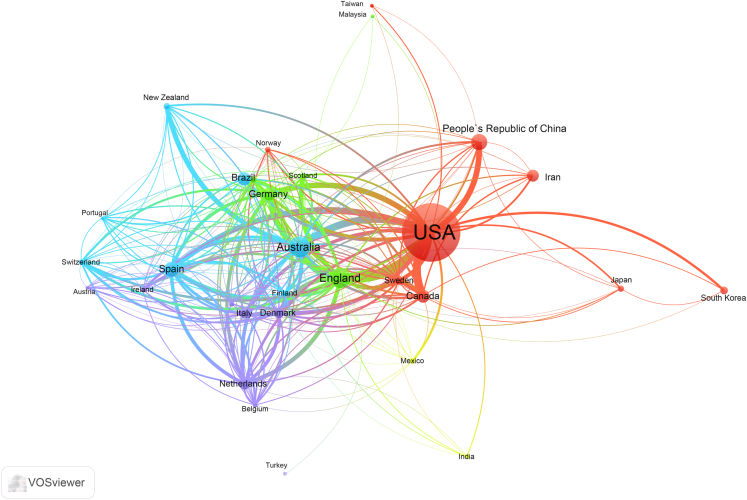
Country/region cooperation network in obesity intervention
The node represents the country/region, the size of the node represents its publications, and the color of the connection between nodes represents the degree of cooperation between the nodes.
Institutional cooperation
More than 5,000 institutions participated in the publication of these articles, of which the top three institutions were Harvard University (184, 4.05%), University Of California System (161, 3.55%) and Pennsylvania Commonwealth System Of Higher Education Pcshe (119, 2.62%). Among the leading publishing institutions, the vast majority were universities and research institutions in developed countries in Europe and America, which exemplified the lagging behind of research in the field in developing nations. In the institutional cooperation network, five dominant cooperation groups were identified — the University of Washington, Columbia University, the Harvard Medical School, the University of Sydney, and the University of Tehran Medical Sciences, as shown in Figure 2 . In general, the cooperation group headed by the University of Washington and the University of Sydney had relatively numerous participating institutions, and internal cooperation was frequent and active; the other three cooperation groups had relatively few internal participating institutions, and the cooperative partners among them were relatively fixed. Moreover, the cooperation group represented by Tehran Medical University had less connections with other cooperation groups, exhibiting a more independent and stable research cooperation.
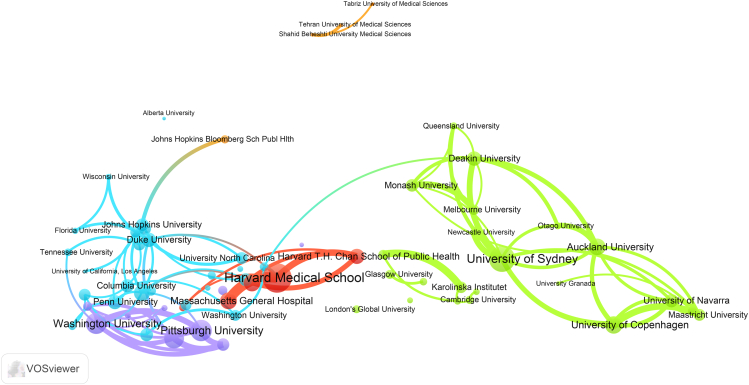
Institutional cooperation network in obesity intervention
The node represents the institutions, the size of the node represents its publications, and the color of the connection between nodes represents the degree of cooperation between the nodes.
Research frontiers of obesity interventions
Based on the above three ways in the “Methods” section, the most cutting-edge research topics in the field of obesity intervention were identified ( Table 1 ). Firstly, we obtained a total of 13,292 research fronts through the Research Fronts in Essential Science Indicators (ESI), and eventually screened 6 fronts related to obesity intervention, which according to the research hotspots, were time-restricted eating, probiotic supplementation, surgical bariatric surgery (Roux-en-Y gastric bypass), Semaglutide, low-carbohydrate diet, environmental (family) intervention (Way 1). Considering citation counts and the authority of the journals in the field where the articles were published, we selected 42 top articles. Among these top articles in the field, 25 discussed the effects of different interventions on obesity. The interventions involve time-restricted eating, a Mediterranean diet, a low-carbohydrate diet, Semaglutide, Bimagrumab, Liraglutide, Metformin, aerobic and resistance exercise, and bariatric surgery (laparoscopic sleeve gastrectomy and Roux-Y-gastric bypass) (Way 2). Meanwhile, we used citespace to perform a collinear analysis on the topics and keywords of 4,541 documents. The co-citation analysis of cited references, cited authors, and cited journals was conducted. Research clusters obtained by clustering showed the research hotspots of obesity intervention are focused on family intervention, exercise intervention, bariatric surgery, wearable devices, smartphone intervention, time-restricted eating, community intervention, self-monitoring, mindfulness intervention, high-intensity intermittent training, and resistance training (Way 3). After reading relevant literature on the above research fronts, we classified and summarized that the research frontiers mainly focused on various obesity interventions for the following: dietary interventions (e.g., intermittent energy restriction, ketogenic diets, probiotics, Mediterranean diet, mindful eating), exercise interventions (high-intensity interval training (HIIT) vs. moderate intensity continuous training (MICT), aerobic exercise vs. resistance physical exercise), pharmacological intervention (Semaglutide, Metformin, Liraglutide), bariatric surgery (Roux-en-Y gastric bypass (RYGB), laparoscopic sleeve gastrectomy (SG), adjustable gastric banding (AGB)), intelligent device-based interventions, environmental, and cognitive interventions. Interestingly, time-restricted eating is the hottest research topic, followed by probiotics and Roux-en-Y gastric bypass. As shown by Figure 3 (thematic map), we can see that the gut microbiota is located in the “Basic and transversal themes” quadrant, where the internal linkages are weakly developed but the external linkages are important and have a great potential for development. The gut microbiota has great development potentiality.
Top topic in research of obesity intervention
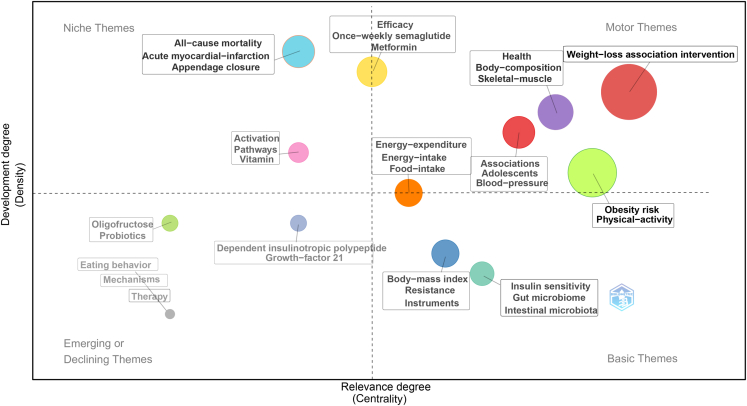
Thematic map of obesity intervention based on Bibliometrix
The first quadrant, characterized by high density and centrality, represents “motor themes” that are well-developed both internally and externally. The second quadrant is labeled as “highly developed-and-isolated themes” as it deals with niche themes. The third quadrant, with low density and centrality, is termed the “emerging-or-declining themes” quadrant. Themes in this quadrant are characterized by weak ties at both internal and external levels. Finally, the “basic-and-transversal themes” quadrant, with low density and high centrality, comprises themes that are weakly developed in terms of internal ties but have important external ties, characterized by high development potentiality.
Dietary interventions
Dietary intervention is the most commonly used measure to improve obesity as well as the most popular direction in obesity intervention research. Research hotspots in the direction of dietary intervention are as follows:1) Intermittent energy restriction (IER): In recent years, there has been an increasing number of researches on the improvement of obesity through IER, primarily focusing on both intermittent fasting (energy restriction) 7 , 8 , 9 and time-restricted eating (meal time restriction). 8 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 Compared to traditional continuous energy restriction (CER), IER patterns generate equivalent weight loss. CER is relatively ineffective in achieving and maintaining weight loss, while IER helps research subjects adhere for longer durations. 8 2) Ketogenic Diets (KD): The ketogenic diet can be used as a quick and effective way to lose weight and reduce abdominal fat in overweight or obese patients. However, some studies suggested that the effect of KD is not due to the loss of appetite but primarily depends on adherence to calorie restriction. Therefore, weight gain and treatment failure are inevitable. 19 , 20 , 21 3) Probiotics: The intake of probiotics has a certain regulatory effect on weight and BMI. In populations with longer treatment durations, there is a greater magnitude of weight loss. Probiotic intervention can improve anthropometric biomarkers and levels of short-chain fatty acids related to human obesity. 22 , 23 , 24 Studies on the application of probiotics in obesity management are valuable. 4) Mediterranean diet: The Mediterranean diet is an effective way to ameliorate obesity and can further reduce the risk of cardiovascular disease. 25 5) Mindful eating: Mindful eating aims at fostering awareness and focuses on eating and on paying attention to hunger and satiety cues. Mindful eating is not only a practical option for weight loss when compared with no intervention controls but also an equivalent alternative to dieting approaches based on limited energy intake and nutrition plans. However, research on mindful eating has shown contradictory and inconsistent results so far. And such studies with long-term follow-up to evaluate the long-term effects of mindful eating are also required in the future. 26 , 27 6) Low carbohydrate diet: Low carbohydrate diet has been one of the hot research directions in recent years to assess the energy consumption of diets with different carbohydrate-fat ratios. Lowering dietary carbohydrate intake increases energy expenditure during weight loss maintenance. This metabolic effect may improve the success of obesity treatment, especially among those with high insulin secretion. 28 , 29
Exercise interventions
Exercise intervention achieves weight loss through increase of energy consumption, which has been the most popular direction in recent years. The research hotspots of exercise intervention are as follows: 1) High-intensity interval training (HIIT) vs. Moderate intensity continuous training (MICT):Most studies suggest that HIIT is similarly effective at losing weight as MICT, and HIIT has recently been recognized as a time-efficient alternative to traditional MICT for the treatment of chronic diseases. 30 , 31 2) aerobic exercise vs. resistance physical exercise: Both aerobic and resistance exercise are effective in treating obesity and its comorbidities. Aerobic exercise is more effective at reducing body fat and improving cardiorespiratory fitness, while resistance exercises are preferrably suitable for muscle strengthening. 13 , 32 , 33 , 34 , 35
Pharmacological interventions
Although lifestyle intervention may be essential to weight loss, some individuals find it difficult to maintain long-term perseverance. Pharmacological weight loss is an important treatment option in addition to lifestyle interventions and bariatric surgery. In recent years, evidence has also suggested that some novel drugs have potential weight loss effects. However, the advantages and disadvantages of existing drugs and potential weight loss drugs are unclear. The efficacy and safety of weight loss drugs have become a hot research direction in this field. Among the multitude of weight-loss drugs, Semaglutide, 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 metformin, 45 , 46 , 47 and liraglutide 48 , 49 , 50 are popular in the study of their effect on obesity. They have positive effects in the treatment of obesity, all of which can lead to weight loss in patients. However, adverse events of varying degrees occur, suggesting that pharmacological interventions may not be suitable for all patients. In obese adolescents, the use of liraglutide (3.0 mg) as an adjuvant treatment resulted in a greater decrease in BMI score and standard deviation compared to placebo. However, a higher incidence of gastrointestinal adverse events was observed with liraglutide, suggesting that this treatment may not be suitable for all patients. 49
Bariatric surgeries
Bariatric surgery is an effective treatment for severe obesity (body mass index≥ 40,or >35 kg/m 2 with comorbidities) that provides rapid and durable improvements in obesity but may increase the risk of postoperative adverse events and postoperative complications. In recent years, Roux-en-Y gastric bypass (RYGB), 51 , 52 , 53 laparoscopic sleeve gastrectomy (SG), 52 , 54 , 55 , 56 , 57 and adjustable gastric banding (AGB) 58 , 59 , 60 , 61 have become the three most commonly used procedures for the treatment of morbid obesity worldwide. Although bariatric surgery is beneficial for patients to lose weight, it may lead to problems such as nutritional deficiencies in patients or the requirement for additional abdominal surgery.

Cognitive remediation therapies
Cognitive remediation therapy is an effective weight loss method that achieves the purpose of treatment through psychological intervention and behavioral guidance. In addition to conventional weight loss methods such as exercise and dietary interventions, psychological interventions such as behavioral therapy, cognitive behavioral therapy, and hypnotherapy have been shown to produce superior long-term effects, 62 , 63 , 64 as a result they have also received attention.
Intelligent device-based interventions
With the rapid development of science and technology, the demand and reliance on the Internet and mobile devices are becoming increasingly stronger, and carrying out obesity intervention through network and artificial intelligence technology has become a hot research field. In recent years, an increasing number of researchers have started to explore the development of mobile devices based on artificial intelligence technology for the management and improvement of obesity. Mobile apps and wearable devices are effective self-regulating tools for weight loss. Smart apps guide users to maintain specific nutritional goals by determining daily energy intake and expenditure and providing users with future meal recommendations. Smart applied interventions have the potential to become a labor-efficient, effective, and low-cost program that can be implemented throughout the clinical setting, especially for childhood weight management, and are a viable and innovative treatment approach that, in addition to standard care, yields superior treatment outcomes than standard treatment alone. 65 , 66 , 67 , 68 , 69 , 70 , 71 Future studies should assess treatment effects with longer follow-ups and larger samples.
Environmental intervention
Losing weight through environmental intervention has also been a research hotspot in recent years. The above-mentioned interventions all directly or indirectly act on individual obese patients, while environmental interventions act on the population as a whole, which is beneficial for national or local government agencies to regulate and control the prevalence of obesity at the macro level. Popular directions for environmental interventions are: 1) Urban planning intervention: Through establishing appropriate distances between parks, trails, supermarkets, convenience stores, and other places of residence and living places, the frequency of activities, shopping frequency, shopping volume, and road energy consumption can have a positive impact on obesity improvement. 72 , 73 , 74 , 75 , 76 , 77 2) Community intervention: improve community obesity through community health promotion and guidance, health activity organization, and exercise equipment optimization. 78 , 79 , 80 , 81 , 82 , 83 , 84 3) Family based intervention: Through family intervention, promote a good health culture, interact with family members, and form good living habits to improve obesity. 85 , 86 , 87 , 88 , 89
In this scoping review, we found that obesity intervention is becoming more prevalent. We summarized and classified research frontiers of intervention into seven categories: dietary interventions (e.g., intermittent energy restriction, ketogenic diets, probiotics, Mediterranean diet, mindful eating), exercise interventions (high-intensity interval training (HIIT) vs. moderate intensity continuous training (MICT), aerobic exercise vs. resistance physical exercise), pharmacological intervention (Semaglutide, Metformin, Liraglutide), bariatric surgery (Roux-en-Y gastric bypass (RYGB), laparoscopic sleeve gastrectomy (SG), adjustable gastric banding (AGB)), intelligent device-based interventions, environmental, and cognitive interventions. Time-restricted eating is the most prevalent, followed by probiotics and Roux-en-Y gastric bypass. The gut microbiota is a very promising topic of research. Although methods such as restricted eating and the use of semaglutide for weight loss have been popular research topics in recent years, they may not necessarily be the most suitable in every situation, suggesting the need to develop more clinical researches/trials for exploring the optimal interventions for different obesity situations.
In recent years, similar studies have also been carried out by bibliometric analysis of obesity-related research status and frontier hot spots. However, earlier studies (including data prior to 2018) have not provided a comprehensive analysis of the research hotspots of obesity intervention, as well as classify and summarize the recent research frontiers in the field. For instance, Ozsoy, Z et al. conducted 2 bibliometric analyses of bariatric surgery and reported that the most advanced surgery was Roux-en-Y gastric bypass, while the most popular surgery was sleeve gastrectomy. 90 , 91 In addition, Paolino, L’s team also conducted a bibliometric analysis of weight loss surgery, concluding that the most common surgery was Roux-en-Y gastric bypass (RYGB), followed by sleeve gastrectomy (SG) and adjustable gastric banding (AGB). 92 Toro-Huamanchumo et al. also conducted a bibliometric analysis of bariatric surgery to analyze the current status of research in this field in Latin America, and countries with the highest output (the number of publications) were Brazil (64.7%) and Chile (14.5%), and countries outside the region were Brazil (64.7%) and Chile (14.5%). Cooperation is primarily with the United States. 93 In addition, Yao et al. conducted a bibliometric analysis of the related research on the role of gut microbiota in obesity. 94 Zhao N`s team searched for research hotspots and trends of obesity in the future through bibliometrics, and concluded that “weight loss surgery” (especially “sleeve gastrectomy”) and “obesity complications” (especially “diabetes,” “metabolic syndrome,” “depression,” and “polycystic ovary syndrome”) most likely maintain the research hotspots of obesity next decades. 95 Obesity intervention is increasingly prevalent, against this situation, our scoping review presents the most comprehensive and elaborate latest summary of obesity intervention to date.
In addition, compared with using bibliometric analysis alone in these above researches, we employed two other approaches to extract and determine research frontiers. We found that using bibliometric analysis alone in the process of clustering makes it difficult to accurately explain the correlation between high-frequency keywords and in turn summarize clear research hotspots. This deficiency can be considerably offset by employing the above two approaches coupled with reading of the literature.
Through analysis of research frontiers in this field, we expect a number of obesity intervention research will be continuously carried out, producing a large number of scientific research results with a high impact, such as gut microbiota, intermittent energy restriction, 96 artificial intelligence device intervention in the era of big data, exercise training of different intensities, comparison between different weight loss drugs, 97 and Roux-en-Y gastric bypass (RYGB). The developed countries and institutions in Europe and the United States will undoubtedly continue to lead the research and exploration in the short term, however, as developing countries are increasingly gaining attention to obesity, we expect an increase in research activity accordingly. Research methods and research hotspots carried out by developed countries such as the European Union and the United States can help stakeholders in developing countries find their own ways to improve interventions for obesity or weight loss. 98
There are also limitations in this study. In the retrieval process, we only considered the database of the core collection of Web of Science, which may lead to omissions in the generalization of the field. However, on the other hand, the core collection of Web of Science has a high reputation in the academic field, and the included journals represent reliable academic quality. Moreover, this study lacked a comparison and summary of obesity intervention for the population of different ages. Hence, research on the frontiers of obesity intervention by age group is worth in-depth exploration.
Conclusions
This study describes the research status and distribution of obesity intervention through bibliometric analysis and comprehensively identifies and summarizes the research hotspots of obesity intervention in three ways. Research on obesity interventions are still in a highly developed stage at present. Among various research topics, time-restricted eating is the hottest research topic, followed by probiotics and Roux-en-Y gastric bypass. In addition, although intervention studies such as intermittent dietary restriction and Roux-en-Y gastric bypass are popular, they are not necessarily most suitable in every situation. More research is required in the future to explore the optimal intervention for different obesity situations, as well as to systematically evaluate the advantages and disadvantages of different interventions. In summary, this study raises awareness and promotes appreciation for research on obesity intervention. It also provides valuable insights for researchers and policymakers to engage in obesity intervention research.
Acknowledgments
We thank Prof. Mingming Zhang for English editing.
Funding: This study was supported by the National Natural Science Foundation of China (Grant No. 71573183) and the 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (Grant No. ZYYC08003).
Author contributions
XS and LZ conceived the study. XS acquired the funding. XS and LZ designed the study. LHZ, SD, and WL developed the search strategy. LZ and LHZ developed and tested the data collection forms. LHZ, YFC, TTJ, and WL acquired the data. LHZ, JP, and WL conducted the analysis and interpreted the data. LHZ and SD drafted the article. LHZ, SD, XS, and LZ critically revised the article. All authors read and approved the final article.
Declaration of interests
The authors declare no competing interests.
Contributor Information
Li Zhao, Email: [email protected].
Xin Sun, Email: [email protected].
- 1. World Health Organization . WHO; 2021. The Detail of Obesity and Overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [ Google Scholar ]
- 2. Blüher M. Obesity: global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019;15:288–298. doi: 10.1038/s41574-019-0176-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Chooi Y.C., Ding C., Magkos F. The epidemiology of obesity. Metab-Clin Exp. 2019;6–10 doi: 10.1016/j.metabol.2018.09.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Pan X.F., Wang L., Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021;9:373–392. doi: 10.1016/S2213-8587(21)00045-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Stuart D. Open bibliometrics and undiscovered public knowledge. Online Inf. Rev. 2018;42:412–418. [ Google Scholar ]
- 6. Cooper I.D. Bibliometrics basics. J. Med. Libr. Assoc. 2015;103:217–218. doi: 10.3163/1536-5050.103.4.013. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Lister N.B., Jebeile H., Truby H., Garnett S.P., Varady K.A., Cowell C.T., Collins C.E., Paxton S.J., Gow M.L., Brown J., et al. Fast track to health - Intermittent energy restriction in adolescents with obesity. A randomised controlled trial study protocol. Obes. Res. Clin. Pract. 2020;14:80–90. doi: 10.1016/j.orcp.2019.11.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Rynders C.A., Thomas E.A., Zaman A., Pan Z., Catenacci V.A., Melanson E.L. Effectiveness of Intermittent Fasting and Time-Restricted Feeding Compared to Continuous Energy Restriction for Weight Loss. Nutrients. 2019;10 doi: 10.3390/nu11102442. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Sundfor T.M., Svendsen M., Tonstad S. Effect of intermittent versus continuous energy restriction on weight loss, maintenance and cardiometabolic risk: A randomized 1-year trial. Nutr. Metabol. Cardiovasc. Dis. 2018;7:698–706. doi: 10.1016/j.numecd.2018.03.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Anton S.D., Lee S.A., Donahoo W.T., McLaren C., Manini T., Leeuwenburgh C., Pahor M. The Effects of Time Restricted Feeding on Overweight, Older Adults: A Pilot Study. Nutrients. 2019;7 doi: 10.3390/nu11071500. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Cienfuegos S., Gabel K., Kalam F., Ezpeleta M., Wiseman E., Pavlou V., Lin S., Oliveira M.L., Varady K.A. Effects of 4-and 6-h Time-Restricted Feeding on Weight and Cardiometabolic Health: A Randomized Controlled Trial in Adults with Obesity. Cell Metab. 2020;32:366–378.e3. doi: 10.1016/j.cmet.2020.06.018. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Lowe D.A., Wu N., Rohdin-Bibby L., Moore A.H., Kelly N., Liu Y.E., Philip E., Vittinghoff E., Heymsfield S.B., Olgin J.E., et al. Effects of Time-Restricted Eating on Weight Loss and Other Metabolic Parameters in Women and Men With Overweight and Obesity: The TREAT Randomized Clinical Trial. JAMA Intern. Med. 2020;180:1491–1499. doi: 10.1001/jamainternmed.2020.4153. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 13. Moro T., Tinsley G., Bianco A., Marcolin G., Pacelli Q.F., Battaglia G., Palma A., Gentil P., Neri M., Paoli A. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J. Transl. Med. 2016;14:1–10. doi: 10.1186/s12967-016-1044-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Parr E.B., Devlin B.L., Radford B.E., Hawley J.A. A Delayed Morning and Earlier Evening Time-Restricted Feeding Protocol for Improving Glycemic Control and Dietary Adherence in Men with Overweight/Obesity: A Randomized Controlled Trial. Nutrients. 2020;2 doi: 10.3390/nu12020505. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Ravussin E., Beyl R.A., Poggiogalle E., Hsia D.S., Peterson C.M. Early Time-Restricted Feeding Reduces Appetite and Increases Fat Oxidation But Does Not Affect Energy Expenditure in Humans. Obesity. 2019;27:1244–1254. doi: 10.1002/oby.22518. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Xie Z., Sun Y., Ye Y., Hu D., Zhang H., He Z., Zhao H., Yang H., Mao Y. Randomized controlled trial for time-restricted eating in healthy volunteers without obesity. Nat. Commun. 2022;13:1003. doi: 10.1038/s41467-022-28662-5. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Thomas E.A., Zaman A., Sloggett K.J., Steinke S., Grau L., Catenacci V.A., Cornier M.A., Rynders C.A. Early time-restricted eating compared with daily caloric restriction: A randomized trial in adults with obesity. Obesity. 2022;30:1027–1038. doi: 10.1002/oby.23420. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Jamshed H., Steger F.L., Bryan D.R., Richman J.S., Warriner A.H., Hanick C.J., Martin C.K., Salvy S.J., Peterson C.M. Effectiveness of Early Time-Restricted Eating for Weight Loss, Fat Loss, and Cardiometabolic Health in Adults With Obesity A Randomized Clinical Trial. JAMA Intern. Med. 2022;182:953–962. doi: 10.1001/jamainternmed.2022.3050. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Casanueva F.F., Castellana M., Bellido D., Trimboli P., Castro A.I., Sajoux I., Rodriguez-Carnero G., Gomez-Arbelaez D., Crujeiras A.B., Martinez-Olmos M.A. Ketogenic diets as treatment of obesity and type 2 diabetes mellitus. Rev. Endocr. Metab. Disord. 2020;21:381–397. doi: 10.1007/s11154-020-09580-7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Di Rosa C., Lattanzi G., Taylor S.F., Manfrini S., Khazrai Y.M. Very low calorie ketogenic diets in overweight and obesity treatment: Effects on anthropometric parameters, body composition, satiety, lipid profile and microbiota. Obes. Res. Clin. Pract. 2020;14:491–503. doi: 10.1016/j.orcp.2020.08.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Kong Z., Sun S., Shi Q., Zhang H., Tong T.K., Nie J. Short-Term Ketogenic Diet Improves Abdominal Obesity in Overweight/Obese Chinese Young Females. Front. Physiol. 2020;11:856. doi: 10.3389/fphys.2020.00856. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Barengolts E., Salim M., Akbar A., Salim F. Probiotics for Prosperity: Is There a Role for Probiotics in the Fight Against Obesity? Review of Meta-Analyses of Randomized Controlled Trials. Nutr. Diet. Suppl. 2020;Volume 12:255–265. [ Google Scholar ]
- 23. Chaiyasut C., Sivamaruthi B.S., Lailerd N., Sirilun S., Khongtan S., Fukngoen P., Peerajan S., Saelee M., Chaiyasut K., Kesika P., et al. Probiotics Supplementation Improves Intestinal Permeability, Obesity Index and Metabolic Biomarkers in Elderly Thai Subjects: A Randomized Controlled Trial. Foods. 2022;3 doi: 10.3390/foods11030268. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Wiciński M., Gębalski J., Gołębiewski J., Malinowski B. Probiotics for the Treatment of Overweight and Obesity in Humans-A Review of Clinical Trials. Microorganisms. 2020;8 doi: 10.3390/microorganisms8081148. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Boque N., Tarro L., Rosi A., Torrell H., Saldana G., Luengo E., Rachman Z., Pires A., Tavares N.T., Pires A.S., et al. Study Protocol of a Multicenter Randomized Controlled Trial to Tackle Obesity through a Mediterranean Diet vs. a Traditional Low-Fat Diet in Adolescents: The MED4Youth Study. Int. J. Environ. Res. Publ. Health. 2021;9 doi: 10.3390/ijerph18094841. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Artiles R.F., Staub K., Aldakak L., Eppenberger P., Ruehli F., Bender N. Mindful eating and common diet programs lower body weight similarly: Systematic review and meta-analysis. Obes. Rev. 2019;11:1619–1627. doi: 10.1111/obr.12918. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Kumar S., Croghan I.T., Biggs B.K., Croghan K., Prissel R., Fuehrer D., Donelan-Dunlap B., Sood A. Family-Based Mindful Eating Intervention in Adolescents with Obesity: A Pilot Randomized Clinical Trial. Children-Basel. 2018;7 doi: 10.3390/children5070093. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Ebbeling C.B., Feldman H.A., Klein G.L., Wong J.M.W., Bielak L., Steltz S.K., Luoto P.K., Wolfe R.R., Wong W.W., Ludwig D.S. Effects of a low carbohydrate diet on energy expenditure during weight loss maintenance: randomized trial. BMJ Br. Med. J. (Clin. Res. Ed.) 2018;363 doi: 10.1136/bmj.k4583. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Ebbeling C.B., Knapp A., Johnson A., Wong J.M.W., Greco K.F., Ma C., Mora S., Ludwig D.S. Effects of a low-carbohydrate diet on insulin-resistant dyslipoproteinemia-a randomized controlled feeding trial. Am. J. Clin. Nutr. 2022;115:154–162. doi: 10.1093/ajcn/nqab287. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. D'Amuri A., Sanz J.M., Capatti E., Di Vece F., Vaccari F., Lazzer S., Zuliani G., Dalla Nora E., Passaro A. Effectiveness of high-intensity interval training for weight loss in adults with obesity: a randomised controlled non-inferiority trial. Bmj Open Sport & Exercise Medicine. 2021;3 doi: 10.1136/bmjsem-2020-001021. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Engel F.A., Oestreich J., Donath L., Kunz P., Sperlich B. High-Intensity Interval Training in the sports therapy of overweight and obese adolescents: A review. Bewegungstherap. Gesundheitssport. 2019;2:66–78. [ Google Scholar ]
- 32. Brellenthin A.G., Lee D-c, Bennie J.A., Sui X., Blair S.N. Resistance exercise, alone and in combination with aerobic exercise, and obesity in Dallas, Texas, US: A prospective cohort study. PLoS Med. 2021;6 doi: 10.1371/journal.pmed.1003687. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 33. Dieli-Conwright C.M., Courneya K.S., Demark-Wahnefried W., Sami N., Lee K., Buchanan T.A., Spicer D.V., Tripathy D., Bernstein L., Mortimer J.E. Effects of Aerobic and Resistance Exercise on Metabolic Syndrome, Sarcopenic Obesity, and Circulating Biomarkers in Overweight or Obese Survivors of Breast Cancer: A Randomized Controlled Trial. J. Clin. Oncol. 2018;36:875–883. doi: 10.1200/JCO.2017.75.7526. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Mitsuno T., Shinohara Y., editors. 9th International Conference on Applied Human Factors and Ergonomics (AHFE)/International Conference on Healthcare and Medical Devices; 2018 2019Jul 21-25; Orlando, FL. 2019. Most Effective Enforced Exercise Time for Aerobic Exercise to Burn Body Fat. [ Google Scholar ]
- 35. Said M.A., Abdelmoneem M., Almaqhawi A., Hamid Kotob A.A., Alibrahim M.C., Bougmiza I. Multidisciplinary approach to obesity: Aerobic or resistance physical exercise? J. Exerc. Sci. Fit. 2018;16:118–123. doi: 10.1016/j.jesf.2018.11.001. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Chao A.M., Tronieri J.S., Amaro A., Wadden T.A. Trends in Cardiovascular Medicine. 2021. Semaglutide for the treatment of obesity. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Christou G.A., Katsiki N., Blundell J., Fruhbeck G., Kiortsis D.N. Semaglutide as a promising antiobesity drug. Obes. Rev. 2019;20:805–815. doi: 10.1111/obr.12839. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Davies M., Færch L., Jeppesen O.K., Pakseresht A., Pedersen S.D., Perreault L., Rosenstock J., Shimomura I., Viljoen A., Wadden T.A., et al. Semaglutide 2·4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet (London, England) 2021;10278:971–984. doi: 10.1016/S0140-6736(21)00213-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Javor E., Lucijanić M., Skelin M. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N. Engl. J. Med. 2021;385:e4. doi: 10.1056/NEJMc2106918. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Rubino D., Abrahamsson N., Davies M., Hesse D., Greenway F.L., Jensen C., Lingvay I., Mosenzon O., Rosenstock J., Rubio M.A., et al. Effect of Continued Weekly Subcutaneous Semaglutide vs Placebo on Weight Loss Maintenance in Adults With Overweight or Obesity: The STEP 4 Randomized Clinical Trial. JAMA. 2021;325:1414–1425. doi: 10.1001/jama.2021.3224. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Wadden T.A., Bailey T.S., Billings L.K., Davies M., Frias J.P., Koroleva A., Lingvay I., O'Neil P.M., Rubino D.M., Skovgaard D., et al. Effect of Subcutaneous Semaglutide vs Placebo as an Adjunct to Intensive Behavioral Therapy on Body Weight in Adults With Overweight or Obesity: The STEP 3 Randomized Clinical Trial. JAMA. 2021;325:1403–1413. doi: 10.1001/jama.2021.1831. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Wilding J.P.H., Batterham R.L., Calanna S., Davies M., Van Gaal L.F., Lingvay I., McGowan B.M., Rosenstock J., Tran M.T.D., Wadden T.A., et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N. Engl. J. Med. 2021;384:989–1002. doi: 10.1056/NEJMoa2032183. [ DOI ] [ PubMed ] [ Google Scholar ]
- 43. Rubino D.M., Greenway F.L., Khalid U., O'Neil P.M., Rosenstock J., Sørrig R., Wadden T.A., Wizert A., Garvey W.T., STEP 8 Investigators Effect of Weekly Subcutaneous Semaglutide vs Daily Liraglutide on Body Weight in Adults With Overweight or Obesity Without Diabetes The STEP 8 Randomized Clinical Trial. JAMA-J Am Med Assoc. 2022;327:138–150. doi: 10.1001/jama.2021.23619. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Kadowaki T., Isendahl J., Khalid U., Lee S.Y., Nishida T., Ogawa W., Tobe K., Yamauchi T., Lim S., STEP 6 investigators Semaglutide once a week in adults with overweight or obesity, with or without type 2 diabetes in an east Asian population (STEP 6): a randomised, double-blind, double-dummy, placebo-controlled, phase 3a trial. Lancet Diabetes Endocrinol. 2022;10:193–206. doi: 10.1016/S2213-8587(22)00008-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Chukir T., Mandel L., Tchang B.G., Al-Mulla N.A., Igel L.I., Kumar R.B., Waitman J., Aronne L.J., Shukla A.P. Metformin-induced weight loss in patients with or without type 2 diabetes/prediabetes: A retrospective cohort study. Obes. Res. Clin. Pract. 2021;15:64–68. doi: 10.1016/j.orcp.2020.12.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Hyer S., Balani J., Shehata H. Metformin in Pregnancy: Mechanisms and Clinical Applications. Int. J. Mol. Sci. 2018;7 doi: 10.3390/ijms19071954. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Warnakulasuriya L.S., Fernando M.M.A., Adikaram A.V.N., Thawfeek A.R.M., Anurasiri W.-M.L., Silva R.R., Sirasa M.S.F., Rytter E., Forslund A.H., Samaranayake D.L., Wickramasinghe V.P. Metformin in the Management of Childhood Obesity: A Randomized Control Trial. Child. Obes. 2018;14:553–565. doi: 10.1089/chi.2018.0043. [ DOI ] [ PubMed ] [ Google Scholar ]
- 48. Alruwaili H., Dehestani B., le Roux C.W. Clinical Impact of Liraglutide as a Treatment of Obesity. Clin. Pharmacol. 2021;13:53–60. doi: 10.2147/CPAA.S276085. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 49. Kelly A.S., Auerbach P., Barrientos-Perez M., Gies I., Hale P.M., Marcus C., Mastrandrea L.D., Prabhu N., Arslanian S., NN8022-4180 Trial Investigators A Randomized, Controlled Trial of Liraglutide for Adolescents with Obesity. N. Engl. J. Med. 2020;382:2117–2128. doi: 10.1056/NEJMoa1916038. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Lin C.-H., Shao L., Zhang Y.-M., Tu Y.-J., Zhang Y., Tomlinson B., Chan P., Liu Z. An evaluation of liraglutide including its efficacy and safety for the treatment of obesity. Expert Opin. Pharmacother. 2020;21:275–285. doi: 10.1080/14656566.2019.1695779. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Guimarães M., Osório C., Silva D., Almeida R.F., Reis A., Cardoso S., Pereira S.S., Monteiro M.P., Nora M. How Sustained is Roux-en-Y Gastric Bypass Long-term Efficacy? Roux-en-Y Gastric Bypass efficacy. Obes. Surg. 2021;31:3623–3629. doi: 10.1007/s11695-021-05458-y. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 52. Olbers T., Beamish A.J., Gronowitz E., Flodmark C.-E., Dahlgren J., Bruze G., Ekbom K., Friberg P., Göthberg G., Järvholm K., et al. Laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity (AMOS): a prospective, 5-year, Swedish nationwide study. Lancet Diabetes Endocrinol. 2017;5:174–183. doi: 10.1016/S2213-8587(16)30424-7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 53. Sobhani Z., Amini M., Zarnaghash M., Foroutan H.R., Mojab S.V., Khazraei H., Hosseini S.V. Self-management Behaviors and Anthropometric Indices after Roux-en-Y Gastric Bypass. World J. Surg. 2021;45:1812–1817. doi: 10.1007/s00268-021-05959-y. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. Dargan D., Dolgunov D., Soe K.T., Er P., Naseer F., Lomanto D., So J.B., Shabbir A. Laparoscopic sleeve gastrectomy for morbidly obese adolescents in Singapore. Singapore Med. J. 2018;59:98–103. doi: 10.11622/smedj.2017086. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 55. El Ghazeery M., Elsawaf M., Ashour M., Metwaly M., Hashish M. One-year outcome of laparoscopic sleeve gastrectomy in morbidly obese adolescents. Annals of Pediatric Surgery. 2021;1 [ Google Scholar ]
- 56. Khoursheed M., Al-Bader I., Mouzannar A., Ashraf A., Al-Haddad A., Sayed A., Alsalim A., Fingerhut A. Laparoscopic Sleeve Gastrectomy for Morbid Obesity in Kuwaiti Adolescents. Bariatr. Surg. Pract. Patient Care. 2019;14:68–73. [ Google Scholar ]
- 57. Lainas P., De Filippo G., Di Giuro G., Mikhael R., Bougneres P., Dagher I. Laparoscopic Sleeve Gastrectomy for Adolescents Under 18 Years Old with Severe Obesity. Obes. Surg. 2020;30:267–273. doi: 10.1007/s11695-019-04150-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Musella M., Bruni V., Greco F., Raffaelli M., Lucchese M., Susa A., De Luca M., Vuolo G., Manno E., Vitiello A., et al. Conversion from laparoscopic adjustable gastric banding (LAGB) and laparoscopic sleeve gastrectomy (LSG) to one anastomosis gastric bypass (OAGB): preliminary data from a multicenter retrospective study. Surg. Obes. Relat. Dis. 2019;15:1332–1339. doi: 10.1016/j.soard.2019.05.026. [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. O'Brien P.E., Hindle A., Brennan L., Skinner S., Burton P., Smith A., Crosthwaite G., Brown W. Long-Term Outcomes After Bariatric Surgery: a Systematic Review and Meta-analysis of Weight Loss at 10 or More Years for All Bariatric Procedures and a Single-Centre Review of 20-Year Outcomes After Adjustable Gastric Banding. Obes. Surg. 2019;1:3–14. doi: 10.1007/s11695-018-3525-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 60. Surve A., Zaveri H., Cottam D., Cottam A., Cottam S., Belnap L., Medlin W., Richards C. Laparoscopic stomach intestinal pylorus-sparing surgery as a revisional option after failed adjustable gastric banding: a report of 27 cases with 36-month follow-up. Surg. Obes. Relat. Dis. 2018;14:1139–1148. doi: 10.1016/j.soard.2018.05.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 61. Yu E.W., Kim S.C., Sturgeon D.J., Lindeman K.G., Weissman J.S. Fracture Risk After Roux-en-Y Gastric Bypass vs Adjustable Gastric Banding Among Medicare Beneficiaries. JAMA Surg. 2019;154:746–753. doi: 10.1001/jamasurg.2019.1157. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 62. Storman D., Świerz M.J., Storman M., Jasińska K.W., Jemioło P., Bała M.M. Psychological Interventions and Bariatric Surgery among People with Clinically Severe Obesity-A Systematic Review with Bayesian Meta-Analysis. Nutrients. 2022;8 doi: 10.3390/nu14081592. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 63. Shaw K., O'Rourke P., Del Mar C., Kenardy J. Psychological interventions for overweight or obesity. Cochrane Database Syst. Rev. 2005;2 doi: 10.1002/14651858.CD003818.pub2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Brennan L., Murphy K.D., Shaw K.A., McKenzie J.E. WITHDRAWN: Psychological interventions for overweight or obesity. Cochrane Database Syst. Rev. 2014;2014 doi: 10.1002/14651858.CD003818.pub3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 65. Johansson L., Hagman E., Danielsson P. A novel interactive mobile health support system for pediatric obesity treatment: a randomized controlled feasibility trial. BMC Pediatr. 2020;1 doi: 10.1186/s12887-020-02338-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 66. Langarizadeh M., Sadeghi M., As'habi A., Rahmati P., Sheikhtaheri A. Mobile apps for weight management in children and adolescents; An updated systematic review. Patient Educ. Counsel. 2021;9:2181–2188. doi: 10.1016/j.pec.2021.01.035. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Sefa-Yeboah S.M., Osei Annor K., Koomson V.J., Saalia F.K., Steiner-Asiedu M., Mills G.A. International Journal of Telemedicine and Applications. 2021. Development of a Mobile Application Platform for Self-Management of Obesity Using Artificial Intelligence Techniques. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 68. Tripicchio G.L., Kay M., Herring S., Cos T., Bresnahan C., Gartner D., Sosinsky L.S., Bass S.B. Development and Preliminary Feasibility of iByte4Health: A Mobile Health (mHealth) Pediatric Obesity Prevention Intervention to Engage Parents with Low-Income of Children 2-9 Years. Nutrients. 2021;12 doi: 10.3390/nu13124240. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 69. Vidmar A.P., Salvy S.J., Pretlow R., Mittelman S.D., Wee C.P., Fink C., Steven Fox D., Raymond J.K. An addiction-based mobile health weight loss intervention: protocol of a randomized controlled trial. Contemp. Clin. Trials. 2019;78:11–19. doi: 10.1016/j.cct.2019.01.008. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 70. Wang E., Abrahamson K., Liu P.J., Ahmed A. Can Mobile Technology Improve Weight Loss in Overweight Adults? A Systematic Review. West. J. Nurs. Res. 2020;42:747–759. doi: 10.1177/0193945919888224. [ DOI ] [ PubMed ] [ Google Scholar ]
- 71. Yau K.W., Tang T.S., Gorges M., Pinkney S., Kim A.D., Kalia A., Amed S. Effectiveness of Mobile Apps in Promoting Healthy Behavior Changes and Preventing Obesity in Children: Systematic Review. Jmir Pediatrics and Parenting. 2022;1 doi: 10.2196/34967. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 72. Jia P., Luo M.Y., Li Y.M., Zheng J.S., Xiao Q., Luo J.Y. Fast-food restaurant, unhealthy eating, and childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2021;22:e12944. doi: 10.1111/obr.12944. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 73. Jia P., Zou Y.X., Wu Z.F., Zhang D., Wu T., Smith M., Xiao Q. Street connectivity, physical activity, and childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2021;22 doi: 10.1111/obr.12943. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 74. Pan X.F., Zhao L., Luo J.Y., Li Y.H., Zhang L., Wu T., Smith M., Dai S.Q., Jia P. Access to bike lanes and childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2021;22 doi: 10.1111/obr.13042. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 75. Wang Z., Zhao L., Huang Q., Hong A., Yu C., Xiao Q., Zou B., Ji S.N., Zhang L.H., Zou K., et al. Traffic-related environmental factors and childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2021;22 doi: 10.1111/obr.12995. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 76. Xin J.G., Zhao L., Wu T., Zhang L.H., Li Y., Xue H., Xiao Q., Wang R.O., Xu P.Y., Visscher T., et al. Association between access to convenience stores and childhood obesity: A systematic review. Obes. Rev. 2021;22 doi: 10.1111/obr.12908. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 77. Zhang X., Zhang M., Zhao Z., Huang Z., Deng Q., Li Y., Pan A., Li C., Chen Z., Zhou M., et al. Geographic Variation in Prevalence of Adult Obesity in China: Results From the 2013-2014 National Chronic Disease and Risk Factor Surveillance. Ann. Intern. Med. 2020;172:291. doi: 10.7326/M19-0477. [ DOI ] [ PubMed ] [ Google Scholar ]
- 78. Jia P., Xue H., Cheng X., Wang Y.F. Effects of school neighborhood food environments on childhood obesity at multiple scales: a longitudinal kindergarten cohort study in the USA. BMC Med. 2019;17:99. doi: 10.1186/s12916-019-1329-2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 79. Jia P., Xue H., Cheng X., Wang Y., Wang Y. Association of neighborhood built environments with childhood obesity: Evidence from a 9-year longitudinal, nationally representative survey in the US. Environ. Int. 2019;128:158–164. doi: 10.1016/j.envint.2019.03.067. [ DOI ] [ PubMed ] [ Google Scholar ]
- 80. Hoffman J., Frerichs L., Story M., Jones J., Gaskin K., Apple A., Skinner A., Armstrong S. An Integrated Clinic-Community Partnership for Child Obesity Treatment: A Randomized Pilot Trial. Pediatrics. 2018;1 doi: 10.1542/peds.2017-1444. [ DOI ] [ PubMed ] [ Google Scholar ]
- 81. Huang W.Z., Yang B.Y., Yu H.Y., Bloom M.S., Markevych I., Heinrich J., Knibbs L.D., Leskinen A., Dharmage S.C., Jalaludin B., et al. Association between community greenness and obesity in urban-dwelling Chinese adults. Sci. Total Environ. 2020;702:135040. doi: 10.1016/j.scitotenv.2019.135040. [ DOI ] [ PubMed ] [ Google Scholar ]
- 82. Korn A.R., Hennessy E., Tovar A., Finn C., Hammond R.A., Economos C.D. Engaging Coalitions in Community-Based Childhood Obesity Prevention Interventions: A Mixed Methods Assessment. Child. Obes. 2018;14:537–552. doi: 10.1089/chi.2018.0032. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 83. Schroeder K., McCormick R., Perez A., Lipman T.H. The role and impact of community health workers in childhood obesity interventions: a systematic review and meta-analysis. Obes. Rev. 2018;19:1371–1384. doi: 10.1111/obr.12714. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 84. Strauss W.J., Nagaraja J., Landgraf A.J., Arteaga S.S., Fawcett S.B., Ritchie L.D., John L.V., Gregoriou M., Frongillo E.A., Loria C.M., et al. The longitudinal relationship between community programmes and policies to prevent childhood obesity and BMI in children: the Healthy Communities Study. Pediatr. Obes. 2018;13:82–92. doi: 10.1111/ijpo.12266. [ DOI ] [ PubMed ] [ Google Scholar ]
- 85. Davison K.K., Kitos N., Aftosmes-Tobio A., Ash T., Agaronov A., Sepulveda M., Haines J. The forgotten parent: Fathers' representation in family interventions to prevent childhood obesity. Prev. Med. 2018;111:170–176. doi: 10.1016/j.ypmed.2018.02.029. [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. Haines J., Douglas S., Mirotta J.A., O'Kane C., Breau R., Walton K., Krystia O., Chamoun E., Annis A., Darlington G.A., et al. Guelph Family Health Study: pilot study of a home-based obesity prevention intervention. Can J Public Health-Rev Can Sante Publ. 2018;109:549–560. doi: 10.17269/s41997-018-0072-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 87. Hansen T.V., Vik A., Serhan C.N. The Protectin Family of Specialized Pro-resolving Mediators: Potent Immunoresolvents Enabling Innovative Approaches to Target Obesity and Diabetes. Front. Pharmacol. 2019;9:1582. doi: 10.3389/fphar.2018.01582. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 88. Pratt K.J., Skelton J.A. Family Functioning and Childhood Obesity Treatment: A Family Systems Theory-Informed Approach. Acad. Pediatr. 2018;18:620–627. doi: 10.1016/j.acap.2018.04.001. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 89. Smith J.D., Berkel C., Jordan N., Atkins D.C., Narayanan S.S., Gallo C., Grimm K.J., Dishion T.J., Mauricio A.M., Rudo-Stern J., et al. An individually tailored family-centered intervention for pediatric obesity in primary care: study protocol of a randomized type II hybrid effectiveness-implementation trial (Raising Healthy Children study) Implement. Sci. 2018;13:11. doi: 10.1186/s13012-017-0697-2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 90. Ozsoy Z., Demir E. Which Bariatric Procedure Is the Most Popular in the World? A Bibliometric Comparison. Obes. Surg. 2018;28:2339–2352. doi: 10.1007/s11695-018-3163-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 91. Ozsoy Z., Demir E. The Evolution of Bariatric Surgery Publications and Global Productivity: A Bibliometric Analysis. Obes. Surg. 2018;28:1117–1129. doi: 10.1007/s11695-017-2982-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 92. Paolino L., Pravettoni R., Epaud S., Ortala M., Lazzati A. Comparison of Surgical Activity and Scientific Publications in Bariatric Surgery: an Epidemiological and Bibliometric Analysis. Obes. Surg. 2020;30:3822–3830. doi: 10.1007/s11695-020-04703-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 93. Toro-Huamanchumo C.J., Morán-Mariños C., Salazar-Alarcon J.L., Barros-Sevillano S., Huamanchumo-Suyon M.E., Salinas-Sedo G. Latin American Research on Bariatric Surgery: a Bibliometric Study. Obes. Surg. 2021;31:1869–1876. doi: 10.1007/s11695-020-05058-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 94. Yao H.Q., Wan J.Y., Wang C.Z., Li L.R., Wang J., Li Y.S., Huang W.H., Zeng J.X., Wang Q., Yuan C.S. Bibliometric analysis of research on the role of intestinal microbiota in obesity. PeerJ. 2018;20 doi: 10.7717/peerj.5091. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 95. Zhao N., Tao K.X., Wang G.B., Xia Z.F. Global obesity research trends during 1999 to 2017 A bibliometric analysis. Medicine (Baltim.) 2019;4:7. doi: 10.1097/MD.0000000000014132. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 96. Liu D., Huang Y., Huang C., Yang S., Wei X., Zhang P., Guo D., Lin J., Xu B., Li C., et al. Calorie Restriction with or without Time-Restricted Eating in Weight Loss. N. Engl. J. Med. 2022;386:1495–1504. doi: 10.1056/NEJMoa2114833. [ DOI ] [ PubMed ] [ Google Scholar ]
- 97. Shi Q., Wang Y., Hao Q., Vandvik P.O., Guyatt G., Li J., Chen Z., Xu S., Shen Y., Ge L., et al. Pharmacotherapy for adults with overweight and obesity: a systematic review and network meta-analysis of randomised controlled trials. Lancet (London, England) 2022;399:259–269. doi: 10.1016/S0140-6736(21)01640-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 98. Li J., Shi Q., Gao Q., Pan X.F., Zhao L., He Y., Tian H., Zhu Z., Li S. Obesity pandemic in China: epidemiology, burden, challenges, and opportunities. Chin. Med. J. 2022;135:1328–1330. doi: 10.1097/CM9.0000000000002189. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (3.0 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO