An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Nutritional Assessment
Aditi Kesari ; Julia Y. Noel .
Affiliations
Last Update: April 10, 2023 .
- Continuing Education Activity
Evaluation of nutritional status is critical, either to identify if an individual has nutritional imbalance due to an underlying condition or to assess if an individual is likely to develop a pathological condition due to nutritional imbalance. A detailed, systematic evaluation of a patient's nutritional status conducted by healthcare providers in a team-based setting to diagnose malnutrition and identify underlying pathologies to plan intervention constitutes nutritional assessment. This article provides an overview of nutritional evaluation, including components of nutritional assessment, factors that affect nutritional status, and the role of interprofessional teams involved in managing patients at nutritional risks.
- Explain the significance of nutritional assessment and summarize its components.
- Identify factors that affect the nutritional status of individuals.
- Describe challenges involved in nutritional assessment.
- Summarize the role of interprofessional collaboration in performing the nutritional assessment of patients.
- Introduction
Food and nutrition are basic indispensable needs of humans. Nutrition plays a critical role in maintaining the health and well-being of individuals and is also an essential component of the healthcare delivery system. The nutritional status of individuals affects the clinical outcomes. Essential nutrients are classified into six groups, namely carbohydrates, proteins, lipids, minerals, vitamins, and water.
Nutritional requirements of healthy individuals depend on various factors, such as age, sex, and activity. Hence, recommended values of dietary intakes vary for each group of individuals. In the United States, the Food and Nutrition Board of the Institutes of Medicine (IOM) under the National Academy of Sciences issues nutrition recommendations for populations throughout the life span called Dietary Reference Intakes (DRIs). [1]
An imbalance in nutritional intake leads to malnutrition. The word ‘malnutrition’ is defined in multiple ways, and there is still no consensus. [2] Traditionally, the term malnutrition has been used in the context of lack of energy intake or deficiencies of nutrients, under which two main conditions, namely marasmus, and kwashiorkor, are discussed. Marasmus primarily refers to energy or calorie deficiency, whereas kwashiorkor refers to protein deficiency characterized by peripheral edema. [3] [4]
However, the term malnutrition now includes conditions caused by both insufficient as well as excess intake of macronutrients and micronutrients. [5] As per WHO guidelines, malnutrition encompasses three categories, namely,
- Undernutrition (low weight-for-height, low height-for-age, and low weight-for-age),
- Micronutrient (vitamins and minerals) deficiency or excess, and
- Overnutrition (overweight, obesity, and other diet-related health conditions such as type 2 diabetes mellitus, cardiovascular disorders, etc.).
The presentation of malnutrition can be acute, sub-acute, or chronic and may or may not be associated with underlying inflammation. Furthermore, the double burden of malnutrition has also been emphasized in various studies. This involves the dual manifestation of overnutrition and undernutrition, which makes the diagnosis of malnutrition a challenge. [6] [7]
Hence, a comprehensive, multi-faceted evaluation of a patient's nutritional status is warranted. A comprehensive nutritional assessment, however, should be differentiated from nutritional screening. Nutritional screening is done to quickly identify individuals at risk of developing malnutrition. [8]
For example, the mini nutritional assessment (MNA) is used in the geriatric patient population to screen for individuals at risk of malnutrition. This screening tool consists of a questionnaire and has a scoring system that helps identify at-risk individuals. On the other hand, a comprehensive nutritional assessment is performed to evaluate the nutritional status of patients already identified at nutritional risk. Nutritional assessment allows healthcare providers to systematically assess the overall nutritional status of patients, diagnose malnutrition, identify underlying pathologies that lead to malnutrition, and plan necessary interventions.
While performing nutritional assessment, it is important to understand that there is no single best test to evaluate nutritional status. Information should be collected systematically, and an evaluation of nutritional status should be done based on the overall data collected. As per the American Society for Parenteral and Enteral Nutrition (ASPEN) guidelines, a comprehensive nutritional assessment involves a thorough clinical examination (history and physical examination), anthropometric measurements, diagnostic tests, and dietary assessments. [5]
Additional clinical examinations or diagnostic tests may be necessary for different groups of populations and individuals with specific underlying pathology. As per the International Consensus guidelines committee, the diagnosis of malnutrition in adults can be categorized as (i) starvation-related malnutrition (chronic, non-inflammatory), (ii) acute disease or injury-related malnutrition (mild to severe inflammation), or (iii) chronic disease-related malnutrition (chronic mild to moderate inflammation). [9]
Given below are the components of a comprehensive nutritional assessment that need to be performed while evaluating the nutritional status of individuals.
Clinical History: Patients' clinical history is a crucial component of nutritional assessment. Clinical history aims to look for indications of malnutrition and identify underlying factors that may lead to malnutrition or increase the risk of malnutrition.
- Once patient identification markers (name, age, sex) are noted, take a detailed history of chief complaints.
- If not mentioned in chief complaints, ask for other constitutional symptoms, such as fever, fatigue, malaise, loss of appetite, or sleep disturbances. The presence of these symptoms can be an indication of underlying pathologies. For example, fever suggests active infection or inflammation.
- Inquire about the patient’s usual weight and ask if there have been any weight changes. Weight loss of >10% of body weight can signify underlying pathology. Weight gain can be suggestive of various underlying endocrine pathologies. Weight gain can also lead to insulin resistance contributing to metabolic syndrome.
- Ask if there are any symptoms suggestive of malnutrition other than weight changes, such as rashes, sores in the mouth, dryness of skin and eyes, loss of night vision, hair loss, bleeding gums, poor healing of wounds, swelling of extremities, tingling, or numbness.
- Ask about eating habits and dietary preferences. For example, ask about the number of meals eaten in a day, approximate portion sizes, whether they are following any restrictive diets, whether they are vegan or vegetarian, or if they are allergic to any food items. This can help in diagnosing a possible nutritional deficiency. For example, a vegan diet may be associated with vitamin B12 (cobalamin) deficiency. [10] A detailed dietary assessment is also warranted and is discussed below. If patients are on parenteral or enteral diets, they should be interviewed accordingly.
- Ask about any factors affecting food intake, like poor dentition, ulceration in the oral cavity, difficulty in swallowing, loss of appetite, heartburn, nausea, and/or vomiting. Further, inquire about bowel habits, which help assess the general functioning of the gastrointestinal system. Also, ask if there is any abdominal pain, abdominal distention, diarrhea, flatulence, or constipation, which can indicate underlying gastrointestinal pathologies that affect nutritional status.
- Ask about any current major clinical or surgical illnesses, including mental illnesses. Also, ask if they are taking any medications, either prescribed or over the counter. Ask if there is any history of chronic illnesses, hospitalization, trauma, or malignancies. The impact of current or past illnesses on nutritional status is discussed below.
- In female patients, detailed menstrual history should be taken. Amenorrhea in child-bearing aged women can indicate pregnancy, chronic infection, chronic illness, eating disorder, etc., which can affect the nutritional status of patients. History suggestive of menorrhagia can reveal the presence of anemia. Also, a history of contraceptive use is essential. Women on oral contraceptive pills have different nutritional requirements. Oral contraceptive pills have been shown to deplete B vitamins, vitamin C, and some minerals, such as magnesium, selenium, and zinc. [11]
- Next, ask questions related to lifestyle habits (active vs. sedentary), daily physical activities, and exercise routine.
- History about social habits such as drinking, smoking, tobacco consumption, or other non-prescription drugs should also be taken.
- Since socioeconomic conditions can affect nutritional status, request information related to this as well.
- Finally, family history can also be useful for the early diagnosis of conditions that can affect a patient's nutritional status or help identify underlying predisposing conditions.
Dietary Assessment: Dietary assessment is necessary to ensure adequate nutrition and hydration intake. It is advised to consult a qualified registered dietitian-nutritionist (RDN), if available, to obtain a thorough dietary assessment.
- The information can be collected from various sources such as the patients themselves, family members, caregivers, or medical records.
- History about dietary habits, frequency of meals, and serving sizes needs to be collected. As mentioned earlier, details about food preferences, restrictive diets, and allergies should be noted.
- Current nutrient and fluid intake should be recorded. Methods such as the 24-hour recall method, food frequency questionnaire (FFQ), diet charts, observation, etc., can be used. Wearable monitoring devices, phone apps, or nutrition analysis software can be used as aids. [8]
- If patients are on any nutritional supplements, care must be taken to record the frequency and dosage to limit the risk of nutrient insufficiency and toxicity.
- If patients are on parenteral or enteral diets, information on feeding regimens (quantity and frequency) should be noted. Factors affecting these feedings, such as displacement of feeding tubes, site irritation, or infections, should be considered.
Physical examination: The next component of the nutritional assessment is physical examination. The physical examination aims to identify signs of malnutrition and factors affecting nutritional status.
- General condition: General condition and appearance of the patient should be observed. Look for any signs of emaciation. Note whether the patient is conscious, alert, and ambulatory. Make a note of whether a patient is being examined in a hospital or outpatient setting. An initial observation of the patient's cognitive, mental, and emotional status should be noted. Also, note any parenteral or enteral feeding devices being used. A patient's general condition can help determine whether a patient can meet their nutritional needs and/or whether their condition is causing their malnutrition or putting them at a higher risk of nutrition deficiencies.
- Vital signs: Vital signs (body temperature, pulse, blood pressure, and respiratory rate) should be checked. Temperature > 100.4 degrees Fahrenheit or 38 degrees Celsius can signify active inflammation/infection. Hypothermia (temperature < 95 degrees Fahrenheit or 35 degrees Celsius) can be associated with conditions causing impaired nutritional status, such as sepsis, trauma, burns, stroke, alcohol intoxication, and metabolic disorders like hypothyroidism, adrenal insufficiency, and Wernicke encephalopathy. [12] High pulse rates, apart from cardiac conditions, can indicate hyperdynamic circulation. Some causes of hyperdynamic circulation that are associated with altered nutritional status are fever, anemia, pregnancy, hyperthyroidism, septic shock, Beriberi, and anxiety. High blood pressure or hypertension is one of the risk criteria for metabolic syndrome. Abnormal rate and patterns of respiration can be indicative of various pathologies. For example, Kussmaul's breathing is associated with diabetic ketoacidosis (DKA).
- Height and Weight: Measure the height and weight of the patient. Body mass index (BMI) calculated from these variables can help determine whether an individual is undernourished or overnourished. Details about BMI and other anthropometric measurements are discussed later.
- Eyes: Look for pallor, which may be indicative of various nutrient deficiencies (iron, vitamin B12, folic acid, vitamin B6, vitamin C, or protein deficiency), as well as various chronic illnesses. Look for icterus, suggesting metabolic disturbances associated with the hepatobiliary system. The presence of Bitot spots and xerosis is indicative of vitamin A deficiency. Xanthelasmas, yellow-colored plaques on eyelids, can suggest obesity, hypercholesterolemia, or diabetes mellitus.
- Oral cavity and perioral region: Assess the general health of the oral cavity and look for pathologies that can affect the adequate intake of nutrients. Also, look for glossitis, angular stomatitis, and cheilosis, which can indicate vitamin B complex deficiency. Bleeding gums and gingivitis are suggestive of vitamin C deficiency. Again, look for pallor. If an eating disorder is suspected, look for vomiting-related oral damage, for example, discoloration of teeth, loss of enamel, cavities, and enlarged salivary glands. [13] A consultation with a dentist may be helpful. Look for loss of buccal fat pads or sunken facial appearance. This can be associated with various conditions such as eating disorders, marasmus, tuberculosis (TB), or HIV/AIDS.
- Skin: Assess the general health of the skin. Xeroderma (extremely dry skin) can signify vitamin A and/or essential fatty acid deficiencies. Petechia, purpura, and ecchymosis may be associated with vitamin C and vitamin K deficiencies. Vitamin C deficiency can also present with perifollicular hemorrhage. Poorly healed wounds indicate vitamin C, protein, and/or zinc deficiencies. Pigmentation and rashes in sun-exposed areas (around the neck and on extremities in glove and stocking patterns) can be due to niacin deficiency. [14] The yellow-orange discoloration of the skin can be detected in cases of excessive consumption of carotenoids (pigments found in carrots, pumpkin, tomatoes, etc.). Xanthomas, which are localized lipid deposits, can be seen in individuals with obesity, hypercholesterolemia, or diabetes mellitus. Look for loss of subcutaneous adipose tissue in axillary folds, buttocks, and extremities. This can be associated with energy-deficient states like marasmus, TB, HIV, and eating disorders.
- Hair: Various nutrients are required to maintain the health of hair and hair follicles. Dry hair can be a sign of vitamin A or vitamin E deficiency. Biotin deficiency can make hair brittle. Severe undernutrition, especially protein deficiency, can lead to discolored and easily pluckable hair, eventually resulting in hair loss. Rapid hair loss can also be indicative of underlying systemic illnesses.
- Nails: Assess the general health of nails and nailbeds. Dry and brittle nails can be associated with various nutritional deficiencies, such as deficiencies in biotin, zinc, and proteins. Discoloration of nails is another sign of poor nutrition. [15] Koilonychia can be a sign of iron deficiency anemia. While clubbing is associated with many pathologies, it may also be observed with malnutrition, chronic alcohol use disorder, and chronic laxative use, often seen in individuals with eating disorders.
- Extremities: Examine all extremities carefully. Protein or thiamine deficiency can lead to edema. Vitamin B12, thiamine, vitamin E, and vitamin B6 deficiencies can present with paresthesia and muscle weakness. Loss of vibration and position sensation can also be observed in individuals with vitamin B12 and/or vitamin E deficiencies. Patients with diabetes mellitus may also show signs of peripheral neuropathy, foot ulceration, or gangrene. Severe undernutrition, as well as chronic illnesses, can lead to muscle atrophy and wasting. Bowing of lower limbs can be seen in children with vitamin D deficiency rickets.
- Odors: Certain odors can be suggestive of specific disorders or substance use. Detection of fruity acetone odor in patients with ketoacidosis, musty odor in patients with phenylketonuria, sweet burnt sugary odor in patients with Maple syrup disorder, or the smell of alcohol can also be helpful during the examination of patients.
- Functional assessment: It is essential to do a functional assessment of patients. Observe whether patients are ambulatory and whether they can eat and drink with or without assistance. Examine the strength of extremities to determine whether they can perform activities of daily living (ADLs) or other physical activities. Mental assessment is also crucial, along with physical assessment. For example, elderly patients with severe malnutrition may be physically (due to weakness) and mentally (due to dementia) incapable of maintaining healthy nutritional status. Similarly, patients with thiamine deficiency may develop Wernicke encephalopathy and Korsakoff psychosis and may become incapable of meeting their own dietary needs.
- Systemic evaluation: An appropriate systemic examination should be performed based on the history and general examination findings.
Anthropometric Measurements
- Height, weight, and BMI: Measure the weight and height of the patient, as mentioned above. Patients should be advised to avoid wearing heavy garments or shoes while these measurements are taken. Bed or chair scales may be needed if patients are not ambulatory or cannot stand. In pediatric age groups, these parameters are plotted on growth charts to assess growth and nutritional status. BMI (weight in kilograms divided by height in meters squared) is also calculated using these parameters, and the state of nutrition can be assessed. In adults, BMI < 18.5 kg/m^2: underweight; BMI = 18.5 to 24.9 kg/m^2: within normal range; BMI > 24.9 to 29.9 kg/m^2: overweight; and BMI ≥ 30 kg/m^2: obesity. [16]
- Factors such as edema and hydration should be considered while making these determinations, as they can affect the weight and BMI values. BMI cannot differentiate between muscle mass and adipose tissue/fat mass. And finally, BMI does not take into account micronutrient deficiencies.
- Other anthropometric measurements: Circumference (arm, abdomen, and thigh) measurements and skinfold (biceps skinfold, triceps skinfold, subscapular skinfold, and suprailiac skinfold) thickness measurements can also help with the evaluation of nutritional status. Skinfold thickness measurements are considered indicators of energy stores (mainly lipid stores). Circumference measurement, namely midarm circumference (MAC), can be used to derive midarm muscle circumference (MAMC=MAC-3.1414 X triceps skinfold thickness), which is an indicator of protein stores. While these tests can quickly be done at the bedside without additional cost, subjectivity in terms of measurements and the applicability of results across various populations can make these tests less reliable.
- A complete anthropometric assessment may also involve body composition measurements, which are discussed in diagnostic tests.
Diagnostic tests: The next component of the nutritional assessment is diagnostic tests, which are done to validate the results of the clinical presentation.
Laboratory Tests
- Routine clinical tests: Routine clinical tests can help evaluate the patient's overall status (as well as nutritional status). [17] These include serum electrolytes, blood urea nitrogen (BUN), creatinine, blood glucose levels, lipid profile, liver enzymes, and complete blood count. Serum electrolytes and hydration status may be deranged in malnourished individuals. BUN and serum creatinine are also predictors of nitrogen balance along with being indicators of renal function, and lower levels of these can be seen in malnourished patients. Low levels of serum creatinine can be indicative of lower muscle mass. Both BUN and creatinine levels, however, can be affected by hydration levels and kidney function. Elevated blood glucose levels and lipid profile (triglycerides and cholesterol) levels are indicators of metabolic syndrome. Hyperglycemia can also be a nonspecific indicator of the inflammatory response. [18]
- Low cholesterol levels can be seen in undernourished individuals. Low hemoglobin is suggestive of anemia. Lymphocyte functioning and proliferation are affected in chronic malnutrition and may manifest as decreased lymphocyte count. [19] Undernutrition and protein deficiency, in general, lead to impaired immune response. Taken together, an impaired, delayed hypersensitivity response (anergic or no reaction) may be seen in undernourished individuals. For example, malnourished individuals with TB may show an anergic tuberculin skin test. [20]
- Visceral proteins: [21] Levels of visceral proteins such as albumin, prealbumin, transferrin, and retinol-binding protein can help evaluate nutritional status. However, none of these tests alone are specific for detecting malnutrition, and their levels can be affected by multiple factors. For example, low serum albumin levels suggest protein deficiency due to malnutrition and other pathologies that affect the protein status, such as liver cirrhosis or nephrotic syndrome. High levels of serum albumin could be associated with dehydration. Albumin has a long half-life (up to 20 days) and, hence, cannot be used for monitoring frequent changes in nutritional status during refeeding. Prealbumin (or transthyretin), a thyroid hormone carrier, is preferred in such cases as it has a shorter half-life (2 to 3 days), which allows for the detection of acute alterations in nutritional status. Retinol-binding protein is another protein with a very short half-life (12 hours) and can be used for monitoring changes in nutritional status. However, its levels are affected by vitamin A levels. Transferrin, an iron transport protein, is another nutritional indicator as well as an acute phase reactant. It has a half-life of approximately ten days, and its levels are affected by serum iron levels.
- Micronutrient levels: If specific micronutrient deficiencies are suspected, individual micronutrient levels can be measured. For example, levels of B vitamins (thiamine, riboflavin, niacin, pyridoxine, folic acid, B12), vitamins A, C, D, E, and K, iron, zinc, selenium, homocysteine, etc., can be measured. More specific tests such as the Schilling test for B12 deficiency or iron panel to differentiate between different types of anemia can also be performed based on clinical presentation.
- Other non-nutrition-specific markers can also be used; for example, C-reactive protein (CRP) can be used to indicate inflammation. [21]
Body Composition Studies
Apart from laboratory tests, body composition studies can be performed to estimate the body's composition in terms of water, air, muscle, bones, and fat mass.
- Bioelectrical impedance analysis (BIA): This helps analyze the body composition based on the ability of different body tissues to conduct electricity. Conductance is higher in tissues with more water and electrolytes (for example, blood) and less in adipose and bone tissues. This is an easy, non-invasive test that can be done at the bedside using low-cost equipment. However, in patients with extremely high BMI or fluid overload, the results may be less accurate.
- Dual-Energy X-ray absorptiometry (DEXA or DXA): This is a standard method used to determine body composition and is also used as a reference to compare other body composition tests. However, it is expensive, requires a specialized machine, and involves exposure to X-rays. It is more commonly used in clinical research than in routine clinical practice. [22]
- Other tests, such as computed tomography (CT) scan and magnetic resonance imaging (MRI), can also be used to determine body composition but are expensive options for routine nutritional assessment. Body composition, however, can be determined when imaging is done for other diagnostic purposes.
- Issues of Concern
Despite multiple studies on malnutrition and the knowledge that malnutrition affects clinical outcomes, the term malnutrition still has different interpretations and usages. In the consensus statement focusing on undernutrition by the Academy of Nutrition and Dietetics and ASPEN, adult malnutrition was used interchangeably with adult undernutrition for discussion. [23]
Also, there is no single best test that can give a complete picture of an individual's nutritional status. Additionally, various factors may affect the interpretation of individual tests or examinations, or the tests may have some shortcomings. Furthermore, the nutritional status of individuals itself is affected by multiple interdependent factors discussed below. Hence a holistic, team-based approach that takes into consideration overall data from clinical examination, dietary assessment, and diagnostic tests is necessary to determine the comprehensive nutritional status of a patient. At the same time, different nutritional screening or assessment tools may be required for different types of patient populations (i.e., children vs. elderly) or settings (i.e., hospital vs. outpatient).
Specialized tests may also be required in any patient, based on the underlying pathology. Another challenge with nutrition evaluation is dual manifestations of malnutrition, in which overnutrition and undernutrition can coexist. This further complicates the diagnostic process. The entire team of healthcare providers should be aware of these concerns to enhance the outcomes of nutritional screening and assessment.
Factors Affecting Nutritional Status
It is important to consider the following factors affecting the nutritional status of individuals while performing a comprehensive nutritional assessment. It is also crucial to remember that these factors can be interdependent. The factors can be classified as physiological, pathological, and psychosocial factors.
Physiological factors: Physiological factors such as age, sex, growth, pregnancy, and lactation can influence nutritional needs and should be considered while performing a nutritional assessment. For example, as a child grows, its nutritional requirements will increase. The recommended nutritional requirements for male and female children of the same age are equal early in life, but as they approach adolescence, males require additional nutritional intake. On reaching adulthood, the rise in nutritional requirements of individuals plateaus off in their respective ranges. However, the caloric and nutritional needs of females increase during pregnancy and lactation. Hence, along with a balanced diet, a pregnant or lactating mother may also require additional supplementation of micronutrients, such as iron, folic acid, calcium, and vitamin D. [24] Maternal age at the time of pregnancy can further affect these requirements. For example, the calcium requirements of pregnant teens are higher than those of pregnant adults. [25] Physical activity also determines the recommended macronutrient (carbohydrate, protein, and/or fat) nutritional requirements. Individuals with an active lifestyle require higher nutritional needs than individuals with a sedentary lifestyle. Failure to meet the additional nutritional needs in any of the situations mentioned above increases the risk of malnutrition, especially if other health conditions coexist. On the other hand, as age advances, the energy needs of elderly individuals decrease due to less mobility and loss of lean tissue leading to decreased appetite. Factors such as poor dentition, increased prevalence of chronic conditions, and adverse effects of polypharmacy combined with psychosocial factors, like poor socioeconomic conditions or dementia, can further decrease intake of nutritious food, thus leading to impairment of nutritional status. [26]
Pathological factors: While performing nutritional assessment, it is important to understand how underlying pathologies can affect nutritional status. Some of these factors are discussed below.
- Genetics: Genetics play a significant role in maintaining an individual's nutritional status. Genetic predisposition combined with lack of physical activity and a high-energy diet can lead to obesity and metabolic syndrome, thus putting individuals at higher risk of developing cardiometabolic diseases. In various genetic disorders, multiple factors could be responsible for the pathogenesis of malnutrition. For example, in cystic fibrosis, malabsorption of nutrients results from decreased uptake by the intestines and reduced secretion of pancreatic enzymes. This, coupled with increased energy needs, can contribute to malnutrition in these patients. [27] Similarly, many other genetic disorders, such as phenylketonuria, Prader-Willi syndrome, maple syrup urine disease, abetalipoproteinemia, and lysosomal storage disorders, significantly affect the nutritional status of individuals.
- Infections: Malnourished individuals are more susceptible to infections and related complications. Interestingly, both acute and chronic infections adversely affect the nutritional status of individuals and can precipitate malnutrition. For example, in measles, an acute viral infection, severe deterioration of the nutritional status of children is observed due to acute inflammatory response, increased energy needs, and decreased intake of nutrients due to sore throat or oral lesions. The coexistence of malnutrition increases the severity of measles infection, susceptibility to secondary infections, and mortality rate. Measles is also associated with vitamin A deficiency, which can lead to xerosis, keratomalacia, and corneal ulceration, contributing to ophthalmological complications. [28] Chronic infections, such as tuberculosis (TB) and human immunodeficiency virus (HIV) infection, are associated with anorexia and cachexia. The underlying proinflammatory cytokine response and metabolic alterations are mainly responsible for this. [29] Other factors, like the adverse effects of drugs, can also contribute to this, thus aggravating malnutrition. Malnutrition, on the other hand, increases the severity of the infection, leading to a bidirectional relationship between infection and malnutrition. Parasitic infestations also severely affect the nutritional status of individuals. [30] For example, intestinal parasite infestation, such as ascariasis, leads to a deficiency of macronutrients and micronutrients.
- Medical and surgical illnesses: Various medical and surgical illnesses affect the nutritional status of individuals through multiple mechanisms and may lead to malnutrition. An important mechanism that leads to malnutrition in patients with systemic disorders is the underlying inflammatory response. Many conditions like cardiovascular diseases, chronic obstructive pulmonary disorders, rheumatoid arthritis, chronic pancreatitis, neuromuscular disorders, etc., have some underlying chronic inflammatory response, which leads to an altered metabolic state. Another mechanism that could lead to nutritional disturbances is malabsorption. Many gastrointestinal pathologies such as inflammatory bowel disease, pernicious anemia, celiac disease, gastrointestinal obstruction, pancreatitis, and liver cirrhosis can lead to malnutrition through this mechanism. Malabsorption can also occur because of conditions affecting other organ systems. For example, right-sided congestive cardiac failure may be associated with intestinal edema, resulting in malabsorption and malnutrition in these patients. The next mechanism is metabolic disturbances observed in conditions characterized by dysfunction of the liver, gallbladder, and pancreas and endocrine disorders like diabetes mellitus, Cushing syndrome, and hyperthyroidism. Malnutrition also occurs due to decreased nutrient intake or loss of nutrients. Poor intake of nutrients can be seen in local pathologies affecting ingestion of food, as well as diseases that have dementia as one of the clinical features, such as Parkinson and Alzheimer diseases. [31] Recurrent nausea or vomiting, which leads to either decrease in the nutrient intake or loss of nutrients, can be seen in gastrointestinal pathologies, cyclic vomiting syndrome, brain tumors, Meniere disease, allergies, migraines, and motion sickness. Similarly, conditions characterized by recurrent diarrhea or steatorrhea can also be associated with malnutrition due to loss of nutrients. Mental illnesses (also discussed in psychosocial factors) affect nutritional status too. The mental status of these patients, adverse reactions to prescription drugs, loss of appetite as part of the disease process, etc., can all lead to malnutrition in these individuals. [32]
- Surgery: Malnutrition before surgery can increase the risk of complications, including increased need for ICU admission, longer recovery time, infections, and higher rates of morbidity and mortality. Hence, a nutritional assessment before surgery is crucial. Surgery alone can be a risk factor for malnutrition due to various factors, such as pre- and post-operative fasting, hypermetabolism, adverse effects due to drugs, pain, and other factors specific to the type of surgery. [33] [34] [33]
- Trauma: Severe trauma cases, including head injuries, burns, and multiple fractures, can put patients at high risk of malnutrition. The initial acute inflammatory response and increased energy needs following trauma lead to a hypermetabolic phase. [35] This, followed by a prolonged period of immobility, leads to muscle atrophy and protein breakdown, causing additional metabolic disturbances. The severe condition of these patients also affects food intake. Altogether, these factors often lead to malnutrition. Furthermore, malnutrition can adversely affect the recovery phase and increase the risk of complications, thus worsening clinical outcomes. [36]
- Malignancies: Malnutrition in malignancies is multi-factorial. Inflammatory mediators, increased energy needs, adverse effects of drugs/therapy (like mouth ulceration, nausea, and vomiting), mental stress, anxiety, and depression can lead to deterioration of nutritional status. Furthermore, malnutrition can inhibit the effectiveness of therapy and worsen the prognosis of the disease. [37]
- Medications: Adverse effects of various drugs, such as nausea, gastric irritation, or loss of appetite, can contribute to decreased food/nutrient intake. Commonly taken over-the-counter (OTC) drugs, such as NSAIDs, can lead to gastrointestinal irritation. Similarly, iron tablets can also cause gastrointestinal irritation and constipation as side effects. Some medications can lead to specific deficiencies, such as the drug isoniazid, which can lead to vitamin B6 (pyridoxine) deficiency. Hence, detailed drug-related history is needed as some drugs can cause drug-nutrient interactions.
Psychosocial factors: Often, the above-mentioned physiological and pathological factors may coexist with psychosocial elements, resulting in further deterioration of nutritional status and eventually leading to malnutrition.
- Factors such as socioeconomic conditions, natural and man-made calamities, cultural norms, religious beliefs, etc., can affect nutritional intake. Undernutrition is the major concern in impoverished areas, famine-stricken, war zones, or refugee camps. Though it may seem obvious that overnutrition is mainly observed in affluent groups due to access to resources, the relationship between obesity and socioeconomic status is complicated. While undernutrition is one of the outcomes of lower socioeconomic status, paradoxically, individuals from these groups are also susceptible to developing obesity. This is due to limited access to fresh, nutrient-dense, and relatively more expensive food on the one hand and easy availability of less expensive, energy-dense food on the other hand. Malnutrition with dual manifestation may especially be seen in these groups of individuals.
- Other factors such as eating disorders, mental illnesses, and unhealthy diet trends can also drastically affect nutritional status and increase the risk of malnutrition.
- Alcohol and substance use are other major factors that need to be considered. Excessive alcohol consumption affects macronutrient and micronutrient metabolism, leading to nutritional deficiencies. [38] Excessive alcohol consumption is associated with multi-organ tissue injury, which leads to inflammation. Alcohol consumption can also affect fluid balance. Furthermore, patients' food habits with chronic alcohol use disorder may further contribute to malnutrition. Similarly, illicit drugs affect the metabolism of nutrients as well. Substance use also affects patients' food habits and emotional and mental status, potentially contributing to malnutrition.
- Clinical Significance
Imbalanced nutritional status adversely affects the health and wellness of individuals. By evaluating the nutritional status of individuals early on, nutritional screening and assessment allow for timely intervention and thus help maintain the health and wellness of individuals and improve quality of life. Timely interventions, especially in specific groups of individuals, such as infants, growing children, pregnant and lactating mothers, etc., help prevent long-term complications.
Nutritional assessment and intervention together break the vicious cycle between malnutrition and various diseases or conditions, in which malnutrition aggravates a disease/condition, and the disease/condition, in turn, precipitates malnutrition. Breaking this cycle helps in improving clinical outcomes. Nutritional and clinical management based on comprehensive nutritional assessment results in positive healthcare outcomes by reducing the recovery period, hospital length of stay, risk of complications, susceptibility to infections, and mortality associated with clinical and surgical illnesses. The use of standardized, systematic nutrition risk screening and assessment in the clinical setting also helps in reducing overall healthcare costs.
- Enhancing Healthcare Team Outcomes
Malnutrition adversely affects the health status of individuals, clinical outcomes, and overall healthcare costs. Since malnutrition is a public health concern, it should be addressed accordingly. To prevent this condition, efforts should be made at multiple system levels (public health, community, and individual). Establishing sustainable food systems, educating individuals about healthy diets and lifestyles, maintaining governmental and local food assistance programs, and arranging nutritional screening programs at schools, housing shelters, nursing facilities, and retirement homes, are just a few ways to improve nutritional status and reduce the burden of malnutrition on the healthcare system.
From a clinical standpoint, a systematic team-based nutritional evaluation helps detect malnutrition or factors causing it early, which allows for early intervention and better clinical outcomes. This requires the involvement of physicians (generalists and specialty care physicians), nurses, dietitians, nutrition specialists/technicians, pharmacists, dentists, and laboratory personnel. The primary attending physician is responsible for overall patient care. Since nutritional status is an important predictor of healthcare outcomes, the primary attending physician’s involvement in nutritional assessment and intervention is critical.
Nutrition specialists/technicians and dietitians also play vital roles in nutritional assessment. For example, dietetic technicians, registered (DTRs) are qualified to assist with general nutrition screenings and may also assist dietitians and other members of the healthcare team with identifying patients at risk for malnutrition in the clinical setting. Clinical dietitians or RDNs are trained to perform medical nutrition therapy (MNT) using the Nutrition Care Process (NCP), which includes nutrition assessment as the first step in identifying potential nutrition problems in patients, such as the risk factors of malnutrition mentioned throughout this article. Many of the components of nutritional assessment in the NCP are synonymous with those mentioned above.
The five domains of nutrition assessment outlined in the NCP include 1) food or nutrition-related history, 2) biochemical data, medical tests, and procedures, 3) anthropometric measurements, 4) nutrition-focused physical findings, and 5) client history. [39] By being involved in the diagnostic process and contributing to the planning and monitoring of steps of the intervention, nutrition specialists/technicians and dietitians help enhance overall healthcare outcomes.
Nurses also help with early nutritional screening to identify nutrition risk factors and monitor the patient's condition to maintain timely documentation records of clinical status. Pharmacists may also provide information about potential drug side effects or conditions that may impact the risk of malnutrition. They may also provide suggestions to help prevent drug-nutrient interactions that could influence a patient's nutrition status (i.e., antiepileptic drugs and potential impact on vitamin D levels).
Dental professionals can also play a unique role in identifying malnutrition risk factors in patients. For example, a child or adult with multiple dental caries and poor dentition will likely be at higher risk for malnutrition due to limitations with oral intake; a dental professional can assist with alleviating these concerns, thus promoting better overall nutrition. Consultations with specialty physicians may be required not only for the management of underlying conditions but also for the improvement of the nutritional status of patients. Other healthcare team members' services and expert opinions are also essential based on a patient's clinical presentation.
Overall, effective collaboration between each healthcare team member is essential to provide a thorough, comprehensive nutritional assessment. While each collaborating member may not function within the same healthcare system, modern technology and dynamic electronic medical records allow clinicians to communicate remotely to provide better overall care, which can manifest into more detailed nutritional assessment data collection and utilization.
As this article highlights, there are many different components of nutritional assessment, and it would be an overwhelming task for one member of the healthcare team to assume responsibility for performing all of these components alone. Therefore, it is to the benefit of the physicians, nursing staff, and allied health professionals to coordinate the facilitation of obtaining appropriate nutrition assessment data that can be used to enhance healthcare outcomes for patients' health and safety.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Aditi Kesari declares no relevant financial relationships with ineligible companies.
Disclosure: Julia Noel declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Kesari A, Noel JY. Nutritional Assessment. [Updated 2023 Apr 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Marasmus. [StatPearls. 2024] Marasmus. Titi-Lartey OA, Gupta V. StatPearls. 2024 Jan
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. [Cochrane Database Syst Rev. 2022] Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, et al. Cochrane Database Syst Rev. 2022 Feb 1; 2(2022). Epub 2022 Feb 1.
- Review Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment. [Clin Geriatr Med. 2002] Review Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment. Guigoz Y, Lauque S, Vellas BJ. Clin Geriatr Med. 2002 Nov; 18(4):737-57.
- Feeding the critically ill obese patient: a systematic review protocol. [JBI Database System Rev Implem...] Feeding the critically ill obese patient: a systematic review protocol. Secombe P, Harley S, Chapman M, Aromataris E. JBI Database System Rev Implement Rep. 2015 Oct; 13(10):95-109.
- Nutrient reference value: non-communicable disease endpoints--a conference report. [Eur J Nutr. 2016] Nutrient reference value: non-communicable disease endpoints--a conference report. Lupton JR, Blumberg JB, L'Abbe M, LeDoux M, Rice HB, von Schacky C, Yaktine A, Griffiths JC. Eur J Nutr. 2016 Mar; 55 Suppl 1:S1-10.
Recent Activity
- Nutritional Assessment - StatPearls Nutritional Assessment - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Nutritional Assessment Form: Overview and Examples
Nutritional assessment forms are important tools used by dietitians and nutritionists to gather information about a client’s nutritional status, dietary habits, lifestyle, health conditions and history, and anything related to nutrition. The nutritional assessment forms can take the form of a paper document that clients fill out in nutrition clinics, an editable document or PDF file sent by the practitioner, or through online tools like Google Forms. Some professional nutritionist software also provides a means to send such forms as questionnaires .
Lifestyle factors
Nutritionist software questionnaires.
I’m Lucy, a Registered Nutritionist Dietitian. From my student years to several years of working in various nutrition fields, I’ve encountered and used different nutritional assessment forms.
In this article, I’ll share my knowledge about nutrition assessment , and discuss what nutritional assessment forms typically include . I will also highlight the differences among nutrition assessment forms used by nutrition practitioners .
If you read until the end, you can even download free nutritional assessment form PDF and Word documents that you can use or customize according to your needs. A sample online nutrition questionnaire from professional nutrition software is also provided.
What is Nutrition Assessment?
Before we delve into the topic of Nutritional Assessment Forms, it’s important to understand the purpose of these forms. To do this, we need to understand what nutrition assessment is.
Nutrition assessment is a method of gathering vital information to identify nutrition problems and their causes . It involves continually comparing a client’s status against accepted standards or goals and making adjustments as needed. Consequently, this process allows practitioners to formulate a nutrition diagnosis and appropriate intervention.
Nutrition assessment is ongoing and dynamic, enabling practitioners to track changes in behavior, nutritional status, and the effectiveness of interventions over time.
In the Academy of Nutrition and Dietetics website’s Nutrition Care Process guide, terminology for nutrition assessment is categorized as shown below:
- Food/Nutrition-Related History
- Anthropometric Measurements
- Biochemical Data, Medical Tests, and Procedures
- Physical Exam Findings
- Client History
- Assessment, Monitoring and Evaluation Tools
- Etiology Category
- Comparative Standards
- Progress Evaluation
Knowing these categories can assist you in formulating your own customized nutritional assessment form, as they provide the foundational data needed for such forms.
What Does a Nutritional Assessment Forms Include?
A nutrition assessment form typically includes a series of questions covering various aspects of the client’s information. However, depending on their specialization and setting, every nutritionist or dietitian tailors their approach, utilizing similar content but focusing on specific information essential to their client’s needs.

Free Nutritional Assessment Form Template
Now that you know how to create your customized nutritional assessment form, it is still important to have an actual example. This is to help you visualize how nutritional assessment forms look in different modes used by other nutritionists and dietitians, such as PDF, Word Doc, and professional nutritionist software like NutriAdmin .
Nutritional Assessment Form Editable Word Document
When using a Word document for the nutritional assessment form, you can either send it directly to your client via email or print it out to be filled during face-to-face consultations. You can download our free template below:
PDF Form, Nutrition Assessment Form
The PDF form can be useful when you want to print out a nutritional assessment form and have the client write their answers. Additionally, you can download a free PDF generated through NutriAdmin below.
There are several professional nutrition apps that have a feature to send questionnaires to clients, including the nutritional assessment form. Moreover, this feature is available in NutriAdmin. It allows you to send questionnaires to clients through email or the client portal. You can also have it as a widget on your website. Alternatively, you can get the link to your questionnaire and send it to your clients through emails, or messaging apps.
You can try out how the online questionnaire feature in NutriAdmin by clicking the phrase below. To try to fill in the questionnaire, we require your email address. By submitting your email, you agree to receive marketing communications from us. You can unsubscribe at any time. Please note that the data you submit in this form will be destroyed; it is solely for demo purposes.
Learn more about this feature through our Online Customizable Questionnaires page.
Nutritional Assessment Form
Also, if you’re already a NutriAdmin user and want this form added to your account, please drop us an email at [email protected] , and we will add it for you.
The Nutritional Assessment Form is one way to gather client information. While an interview during an initial consultation is crucial, this form can provide an overview of the client’s status. Additionally, it can serve as a guide during the consultation for parts needing clarification and emphasis. It will also serve as a record of your client’s relevant information for future reference.
The content of the form also varies depending on the practitioner’s niche or specialization. This is because every person has a different goal or reason for consulting with a nutritionist or dietitian.
Frequently Asked Questions
A crucial tool for gathering comprehensive information about a client’s dietary habits, health conditions, and nutritional status, enabling personalized dietary recommendations.
It provides a structured method to collect essential data for formulating accurate nutrition diagnoses and interventions.
Details on client’s personal information, dietary intake, nutritional goals, medical history, physical activity levels, and lifestyle factors.
By tailoring questions to meet the specific needs of their client base, focusing on relevant information essential for targeted nutritional guidance.
Nutritional assessment forms vary in format from paper documents to editable PDFs and online questionnaires, with customization options for different professional needs.
They enable dietitians and nutritionists to track changes in clients’ nutritional status and adjust interventions accordingly.
Many nutritionist software platforms offer functionalities to send, manage, and analyze these forms as part of client questionnaires.
They streamline the data collection process, improve client engagement, and enhance the accuracy of nutrition plans.
By providing detailed insights into clients’ dietary habits and preferences, enabling tailored recommendations.
They are instrumental in identifying risk factors for nutritional deficiencies and chronic diseases, allowing for early intervention.
Related Posts

How To Make a Recipe for Meal Planning, The Ultimate Guide
12 mins to read. Learn how to create your own recipes for your meal plans.
Read More »

Personal Training Intake Form
5 mins to read. Are you a personal trainer or fitness coach looking for a streamlined and effective way to gather essential client information? Do…
Food Diary Template: Assess and Track Food Intake
7 mins to read. Discover the benefits of using a food diary to assess and track your clients' food intake. Learn practical tips for maximizing…

24-Hour Diet Recall Form: How to Effectively Assess Your Clients’ Food Intake
7 mins to read. Discover the 24-hour diet recall method and its use in your practice. Learn about its reliability, practical tips, and get a…

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
13 Focused Assessment: Nutritional Assessment
Learning objectives.
At the end of the chapter, the learner will:
- Relate concepts of nutrition and metabolism with GI assessment and elimination.
- Identify patients at risk for developing malnutrition.
- Use nutritional assessment in the provision of health care.
- Document findings using correct medical terminology.
I. Overview of Nutritional Assessment
Proper nutrition is important to maintain health and prevent illness. Health care providers must routinely evaluate patients’ nutritional status and to identify any existing or potential nutritional problems. This allows for appropriate referrals and interventions to be provided.
Various physical conditions can disrupt nutritional absorptions. For example, patients with gastrointestinal problems such as inflammatory bowel disease or liver cirrhosis may experience malnutrition. Those with lung problems might have insufficient oral intake due to breathing difficulties. Diabetes patients often face inadequate glucose homeostasis. Psychiatric disorders or depression can lead to functional impairments that cause poor nutritional intake. Cancer patients may suffer from cancer cachexia and malnutrition, and those in pain might decrease their oral intake.
Many medications can also interfere with nutritional absorptions. D iuretics, f or example, may cause dehydration and electrolyte imbalances. Narcotics and opioids can lead to nausea and vomiting, while anticholinergic drugs may cause dry mouth, affecting food intake.
Malnutrition is defined as “deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients” (WHO, 2021). According to the World Health Organization (WHO), malnutrition encompasses several conditions:
- Undernutrition: Wasting (low weight-for-height), stunting (low height-for-age), and underweight (low weight-for-age).
- Micronutrient-related malnutrition: Deficiencies or excesses in vitamins or minerals.
- Overweight, obesity, and diet-related noncommunicable diseases (NCDs): A body mass index (BMI) over 25 kg/m 2 is considered overweight, and a BMI above 30 kg/m 2 is classified as obesity. Diet-related NCDs include cardiovascular disease, diabetes, and certain cancers (such as liver cancer or oral cancer).
Body Mass Index (BMI) estimates body fat using a person’s weight and height. Research has shown that BMI is highly correlated with many metabolic and cardiovascular diseases (CDC, nd.) and is recommended as the primary screening method for weight control and metabolic health assessment. However, BMI has limitations, as it cannot distinguish between fat and lean body mass or subcutaneous fat. Measuring waist circumference to assess abdominal fat is critical and is strongly associated with NCDs (Yurista et al., 2023).
BMI Calculator
Click the link of BMI Calculator and follow the instructions to calculate your BMI (NHLBI, nd.).
II. Anatomy and Physiology
Digestion begins in the mouth, where chewing and mixing with saliva initiate the breakdown of food. In the stomach, food mixes with gastric juices to produce a mixture called chyme. Chyme then passes into the small intestine, where most digestion takes place. In the small intestine, food is dissolved, and nutrients are absorbed into the body. Unabsorbed wastes are passed down to the colon.
Nutrients are divided into macronutrients and micronutrients . Macronutrients refer to carbohydrates, fats, and proteins that must be consumed daily to produce energy and ensure proper bodily function.
Watch the following short video clip to review digestion in the small intestine.
Micronutrients refer to dietary minerals and vitamins that support the body’s metabolism.
The following short video clip provides information on the essential nutrients for life: minerals and vitamins.
Knowledge Check
III. Medical Terminology
IV. Nutritional Assessment
Nutritional assessment is an ongoing component of daily assessment, especially for patients with nutritional concerns and those at risk for nutritional deficits.
General Assessment for Nutritional Status (Hinkle, 2021)
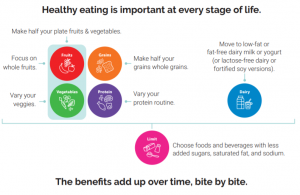
Access additional information to educate patients on healthy dietary patterns. The guidelines were developed by the U.S. Department of Agriculture (USDA) and the U.S. Department of Health and Human Services (HHS) to provide recommendations on healthy eating, promoting health, and preventing chronic illness. These guidelines include recommendations for all stages of life, from birth through older adulthood, as well as for women who are pregnant or breastfeeding.
- Dietary Guidelines for Americans, 2020-2025
V. Documentation of Assessment Findings
Sample Narrative Documentation
Patient was admitted with peptic ulcer this morning. Continues to experience decreased appetite and intermittent epigastric pain, rates 2 on 0-10 pain scale currently. Abdomen soft, distended, and tender to touch. Normal bowel sounds in all 4 quadrants. No bowel movement for 2 days. Pale skin color, warm, dry. Lips pale, oral mucosa moist and intact. Afebrile, BP 110/68, P 100, R 22. Denied shortness of breath. Clear lung sounds bilaterally. No acute distress. Declined pain medication. IV D5W in Left forearm at 50 mL/hr. NPO, wait for the scheduled upper endoscopy procedure.
VI. Related Laboratory and Diagnostic Procedures/ Findings
Nutritional assessment is an ongoing process for hospitalized patients. If assessment findings suggest nutritional concerns, such as inadequate oral intake or poor wound healing, further diagnostic and laboratory tests may be conducted to uncover underlining causes and provide nutritional support.
Certain laboratory results can help determine a patient’s nutritional status. Serum albumin and prealbumin levels are useful for assessing patient’s protein requirements. Electrolytes (such as serum calcium, magnesium, and phosphorous), blood urea nitrogen (BUN), and creatinine can be evaluated to assess fluid volume status and the need for parental nutrition. If diet-related noncommunicable or metabolic diseases are suspected, glucose and lipid levels (total cholesterol, LDL, HDL, and triglycerides) may be assessed. Transferrin, a protein that transports iron through the blood to various tissues and organs, can indicate protein status. Low transferrin levels may signal iron deficiency and anemia. In the evaluation of anemia, a complete blood count (CBC), serum iron level, serum vitamin B12, and folate levels are also checked. Additionally, blood tests for specific vitamin deficiencies may be necessary for patients with gastrointestinal malabsorption (Hinkle, 2021).
Click the link to access additional nutritional assessment OERs: Nutrition .
VII. Learning Exercises
Self learning activity.
Target 3.4 – By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
Indicator 3.4.1 – Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease.
Activity Title: Nutritional Assessment: Unveiling the Path to a Healthier You!
Objectives of this Activity:
You will be able to
- Assess your current eating pattern and gain insight into your nutritional status and overall well-being.
- Identify any imbalances in your diet and take appropriate steps to address them.
Instructions:
- Write out a typical day of meals – breakfast, lunch, dinner, snacks.
- Click MyPlate Plan link: MyPlate Plan.
- Click on the “Start” button.
- Enter your age, sex, height, weight, and physical activity level.
- Click “Calculate food plan” to find your personal plate plan.
- Evaluate your food intake against the recommended plan in the food group amounts – fruits, vegetables, grains, protein, and dairy.
Self-Evaluation Questions:
- What changes do you need to make?
- Explain how you can integrate nutritional knowledge into your daily life and make informed decisions about your diet, ultimately leading to improved overall health outcomes.
VIII. Attribution and References
- Centers for Disease Control and Prevention. Healthy Weight, Nutrition, and Physical Activity: About adult BMI . Available at https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html#InterpretedAdults
- Ernstmeyer, K., & Christman, E. (Eds.). (2021). Open RN Nursing Fundamentals by Chippewa Valley Technical College is licensed under CC BY 4.0.
- Hinkle, J. (2021). Brunner & Suddarth’s Textbook of Medical-surgical Nursing. (15th ed.). Philadelphia, PA: Wolters Kluwer.
- National Heart, Lung, and Blood Institute. Calculate Your Body Mass Index. Available at https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm
- United Nations. Sustainable Development Goals . https://sdgs.un.org/goals
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025 . 9th Edition. December 2020. Available at DietaryGuidelines.gov
- World Health Organization. Malnutrition . 9th June 2021. Available at https://www.who.int/news-room/fact-sheets/detail/malnutrition .
- Yurista, S. R., Eder, R. A., Feeley, M., Kodur, N., Tang, W. H., & Nguyen, C. T. (2023). A closer look at ACC/AHA and ESC guidelines for managing obesity and overweight in adults. Journal of American College of Cardiology Advances, 2(7). https://doi.org/10.1016/j.jacadv.2023.100570
Health Assessment Guide for Nurses Copyright © by Ching-Chuen Feng; Michelle Agostini; and Raquel Bertiz is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book

IMAGES
COMMENTS
The nutrition assessment summary is the last part of each nutrition assessment, and are part of every template for new admissions and follow-ups, as well as quarterlies and annuals (if you’re in LTC). This is where you can write whatever you want, in any kind of format you like. The nutrition assessment summary is as important as you decide ...
Apr 10, 2023 · Food and nutrition are basic indispensable needs of humans. Nutrition plays a critical role in maintaining the health and well-being of individuals and is also an essential component of the healthcare delivery system. The nutritional status of individuals affects the clinical outcomes. Essential nutrients are classified into six groups, namely carbohydrates, proteins, lipids, minerals ...
Jun 21, 2024 · Variations in Creating Nutrition Assessment Forms. Every nutritionist and dietitian creates nutritional assessment forms tailored to their specialization.For instance, a dietitian catering to cancer patients may include questions specific to cancer, such as diagnosis date, type of cancer, stage, treatments, and medications.
Nutrition Assessment and Classification. Introduction NACS USER’S GUIDE MODULE 2, VERSION 2. What is nutrition assessment? Nutrition assessment includes taking anthropometric . measurements and collecting information about a client’s medical history, clinical and biochemical characteristics, dietary practices, current treatment, and food ...
Part 1: Structure of a nutritional assessment Part 2: Phrasing in a nutritional assessment. In this post you’ll: See what a real-life nutrition note example can look like; Learn exactly how to break that down and do it for your patients; Get a cheat sheet with easy phrases that will keep your notes clear, concise, and well written
In nutrition assessment, critical thinking enables the nutrition professional to organize assessment data into a nutrition care plan. It is a process of putting together facts, informed opinions, active listening, and observations to arrive at conclusions that lead to the relevant plan of care.
Nutritional assessment of patients is not an easy procedure. Although, lots of the clinical and laboratory measurements are available for nutritional assessment, all of them have lots of deficiencies. Nutritional assessment is an art more than science. At the current state of the art, in
NR228 Nutrition, Health, and Wellness (Team PURPOSE Required Uniform Assignment: Nutritional Assessment Project) To evaluate, compare, and analyze menus from different agencies and suggest revisions for healthier food choices based on the cultural and age group. Students in a cultural concentration will use that specific cultural
2. This assignment is a required non optional assignment. Failure to submit this assignment will result in failure of the theory portion of the course. No late papers will be accepted. The nutritional assessment constitutes 4% of your grade. The subject of this assessment will be one of the patients you have cared for in the clinical setting. 3.
I. Overview of Nutritional Assessment. Proper nutrition is important to maintain health and prevent illness. Health care providers must routinely evaluate patients’ nutritional status and to identify any existing or potential nutritional problems. This allows for appropriate referrals and interventions to be provided. Various physical ...