An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Geriatric care special needs assessment.
Kiran Ghimire ; Ranjan Dahal .
Affiliations
Last Update: February 20, 2023 .
- Continuing Education Activity
Global life expectancy has been increasing, and so has the population of older patients. Due to multiple comorbidities, the geriatric population has special needs. This activity describes the evaluation of various domains of geriatric assessment and highlights the role of the interprofessional team in the management of older patients.
- Review the common presentation of geriatric patients.
- Identify the unique features in the care of geriatric patients.
- Summarize the management consideration of the older patients.
- Outline how an interprofessional team can coordinate geriatric patients' coordinated evaluation and care to obtain the best outcomes.
- Introduction
The elderly population (age >65 years) is increasing throughout the world, leading to increased hospitalization. There was a 16.7% increase in elderly hospitalization from 2003-2009 in the United States. This rising hospitalization has impacted healthcare services delivery. [1] With the aging population comes a multitude of chronic conditions. It is estimated that 9 out of 10 Americans have at least one chronic condition by age 80. [2]
Due to multiple comorbidities and frailty, the elderly are at increased risk of adverse outcomes with each clinical insult. [1] Besides the common comorbidities such as diabetes and hypertension, older patients can present with atypical presentation too. For example, a patient with sepsis may present without fever, or a patient with Urinary Tract Infection (UTI) may present with confusion. The elderly population varies in cognitive, physical, and social functioning and thus requires different levels of care based on individual needs and functional status. [3] [4]
Geriatric assessment, thus, includes a coordinated approach for the physical, functional, and psychosocial assessment of the elderly and formulate an integrated plan of care. [1]
- Issues of Concern
Issues of concern in geriatric assessment can be broadly divided into the following 4 classes:
- Functional Status
- Vision impairment
- Hearing loss
- Nutrition status
- Fall prevention
Urinary Incontinence
- Osteoporosis and arthritis
- Polypharmacy and Medication Reconciliation
- Sleep and insomnia
- Mood disorder
1. Functional Status
Evaluation of one's ability to perform activities required to live independently comprises functional status assessment. It can be broadly divided into 2 levels - basic activities of daily living (BADL), which includes activities of self-care such as feeding, dressing, bathing, toileting, grooming, controlling bladder and bowel movements, etc. and instrumental activities of daily living (IADL) which includes activities to live independently such as taking medications, shopping, preparing meals, driving/using public transport, handling finances, doing household works, using telephone, etc. Commonly used indices to assess such activities are the Katz index for BADL and the Lawton scale for IADL. Information about functional status can also be achieved by asking open-ended questions about their daily activities. Functional status is directly affected by physical health, so any change in functional status should prompt further evaluation. There are various validated tools to measure functional ability, such as the Vulnerable Elders Scale-13 or Clinical Frailty Scale. [5] [6] Recently, gait speed has also been proposed as a screening tool for functional status. [7] One pooled analysis showed gait speed is associated with better survival for every 0.1 m/s increments. [8]
2. Physical Health
Geriatric assessment should include detailed medical history and physical examination, with particular focus on problems specific to the elderly such as vision, hearing, nutrition, fall prevention, urinary incontinence, osteoporosis, and preventative health.
Preventative Health
Preventative health includes screening for diseases such as diabetes mellitus, hypertension, cancer, etc. Early identification and treatment may be beneficial in diabetes, hypertension as well as in certain malignancies. However, the American Geriatric Society recommended that such screenings be based on patient's preferences, life expectancy, and co-morbid conditions rather than solely on age-based criteria. Older patients may have many co-morbid conditions that can shorten their life, hence the potential benefits of such screening tests and patient's preference for further evaluation and invasive procedure if screened positive should be taken into account before the screening. For the same reason, screening should be focused on treatable conditions which can provide immediate benefit to their quality of life rather than on asymptomatic diseases. [9] Similarly, vaccine-preventable infections such as influenza, pneumonia, herpes zoster, etc., represent major causes of morbidity and mortality in older patients. Hence, most societies recommend following vaccines routinely for older patients: influenza vaccine, pneumococcal vaccine, herpes zoster vaccine and tetanus, Diptheria, and acellular pertussis vaccine. Depending on specific co-morbidities, an older patient may qualify for other vaccines as well. [10] [11]
Visual impairment affects older patients' functional status, especially functions such as driving, preparing meals, managing money, etc. are significantly affected. It is also associated with falls, cognitive decline, and depression in the elderly. [12] Older patients are at increased risk of visual impairment due to age-related decline as well as co-morbid conditions. Common causes of visual impairment in the elderly are cataracts, glaucoma, presbyopia, macular degeneration, diabetic retinopathy, and hypertensive retinopathy. [13] Although studies show an increased association of visual impairment with functional decline, one meta-analysis of 5 randomized controlled trials failed to show any evidence of decreased visual impairment with visual screening in the elderly. [12] [14] The U.S. Preventive Services Task Force (USPSTF) did not find sufficient evidence to recommend routine visual screening in older patients. However, any decline in functional capacity, cognition, or falls should prompt a visual assessment. This can be done with a Snellen chart, questionnaires, or direct fundoscopic examination. In contrast to USPSTF, the American Academy of Ophthalmology recommends comprehensive eye examinations every 1 to 2 years for adults 65 years and older. [15]
Hearing loss is, in fact, the third most common condition in older patients. Like visual impairment, hearing loss is associated with functional decline, poor cognition, and dementia, social isolation, and depression. [16] [17] USPSTF does not recommend routine screening for hearing loss in older patients due to insufficient evidence. However, the decline in cognition, functional capacity, or mood should lead to hearing loss screening. Rapid test such as whispered voice test has shown to be highly sensitive and specific for screening. [18] Providers should be aware of difficulties in communication due to hearing loss and avoid misdiagnosing it as cognitive decline or stroke. Patients who fail the screening test should be referred to an otolaryngologist for possible need of a hearing aid. [19] [16]
Up to 15% of the community-dwelling elderly population is affected by malnutrition, which is associated with a decline in physical health, such as poor wound healing, anemia, immune dysfunction, etc. Poor cognition, functional decline, and an overall increase in mortality. [20] [21] Besides organic causes (chronic medical conditions, malignancy, poor dentition, etc.), various psychosocial causes (depression, alcoholism, isolation, bereavement, etc.) also lead to malnutrition in the elderly. [22] Although there is no single laboratory screening test for this condition, clinical assessment, serial weights on clinic visits, and various validated tools such as Mini Nutritional Assessment (MNA) or Geriatric Nutrition Risk Index (GNRI) can be used for nutritional assessment in older patients. [23] [24] The elderly population at-risk as determined by one of these screening strategies should undergo further evaluation to determine the cause and initiate treatment such as optimizing chronic medical conditions, proper dentition, adequate assistance for physically or mentally disabled patients, and oral supplementation or enteral feeding as needed. [22] [25]
About 28% of older adults report falling at least once in the last year, as per a recent cross-sectional study in the United States. [26] Besides obvious health hazards such as hip fractures and trauma, falls also cause limitations in physical and social activities directly and due to fear of falling indirectly, further leading to functional decline. [27] [28] In the US, the toll on health care cost due to falls is around $50 billion. [29] Therefore, the American Geriatric Society recommends all adults above 65 be screened for falls and instability annually. [30] One meta-analysis of 33 studies evaluating 26 tools for fall risk assessment did not find a single tool to have both high sensitivity and specificity to assess fall risk. [31]
A systematic review of 18 studies reported fall to be multifactorial with the following risk factors - history of falls, gait or balance impairment, orthostatic hypotension, visual impairment, cognitive impairment, impairment in activities of daily living, and medications such as benzodiazepines, antidepressants, diuretics, etc. Of these, the two most predictive risk factors were history of falls and gait or balance impairment. When adjusted for other variables, age was not as important as the aforementioned two risk factors in predicting falls. Hence, a simple approach could be to ask for a history of falls and any abnormality in gait and balance. The patient will be at high risk if he/she answers "yes" to any one of these questions. [32] Due to multifactorial causes, high-risk patients benefit more from a multidisciplinary approach formulating individualized fall prevention strategies, some of which can include exercise programs, optimizing medical conditions, discontinuing medications such as benzodiazepine, environmental safety, and use of assistive devices. [33] [34]
Most studies show the prevalence of urinary incontinence (UI) in the range of 25-45% and rise further with aging. [35] However, UI is not a normal or inevitable consequence of aging. Older patients suffering from UI cannot participate in social activities leading to isolation, increased risk of depression, and functional disability. It can also increase the risk of falls, fractures, affects sexual health, and causes an overall reduction in quality of life. UI can be classified into 5 types - stress, urge, overflow, mixed and functional. Stress incontinence is leakage of urine due to activities that increase abdominal pressure. Urge incontinence is characterized by leakage of urine after a sudden urge to void. Overflow incontinence manifests as frequent small volume leaks, usually due to bladder outlet obstruction or neurological disorders. Functional incontinence refers to incontinence resulting from an inability to use the toilet independently due to functional disability such as cognitive impairment or limited mobility. Mixed incontinence is the combination of 2 or more types of incontinence. [36] [37]
Initial evaluation of incontinence should comprise a non-invasive approach, including detailed medical history, fluid intake assessment, self-voiding diary, etc.; however, complicated cases may necessitate urodynamic studies. A simple and reproducible validated tool to differentiate stress and urge incontinence is 3 Incontinence Questions which comprises questions about urinary leaks. [38] Conservative treatments such as behavioral modification, dietary modification, pelvic floor muscle training, timed voiding, and weight loss should be tried first. Various pharmacological therapies are available for urge incontinence. A systematic review of 13 trials showed anticholinergics as the only pharmacological therapy that decreased urinary leakage in urge incontinence. [39] Devices such as pessaries can be used for incontinence associated with pelvic organ prolapse. Similarly, surgical options such as sling procedures and neuromodulation can be offered to carefully selected patients with incontinence. [36]
Osteoporosis and Arthritis
Osteoporosis and osteopenia are common in the elderly and can lead to fractures even with mild trauma. Increased bone loss due to aging and menopause in women puts older patients and post-menopausal women at high risk of osteoporosis. [40] Screening and diagnosis should be with dual-energy X-ray absorptiometry of the hip and/or spine. Due to their increased risk, USPSTF recommends routine screening of women older than 65 for osteoporosis. [4] Preventive measures in the elderly should include early diagnosis, nutritional supplements with calcium and vitamin D, and fall prevention. [40]
Osteoarthritis (OA) is a major cause of disability and pain in older patients. About 50% of people will have OA changes in knees by age 65, and almost everyone will have at least 1 joint affected with OA by age 75. Evaluation should include ruling out infectious process, rheumatoid arthritis, polymyalgia rheumatic, gout, and pseudogout. A careful history, physical examination, arthrocentesis, laboratory tests, and radiographic imaging may be necessary to come to a diagnosis. Medication such as NSAIDs and acetaminophen are used primarily to manage symptoms as no pharmacological cure is available for OA. Despite early enthusiasm, glucosamine and chondroitin sulfate have not shown to decrease pain in a recent clinical trial. Joint replacement surgery for carefully selected older patients may provide maximum benefit in improving the quality of life. [41]
3. Polypharmacy
Patients older than 65 use more than 30% of all prescribed medication in the U.S. [42] Polypharmacy in the elderly is multifactorial - multiple comorbidities, multiple specialties on board, multiple hospitalization and transition of care, self-medication, prescription cascade, and cognitive decline in the elderly contribute to polypharmacy. [43] [44]
Taking multiple medications can cause serious adverse effects due to the drug itself, drug-drug interaction, and drug-disease interaction. [42] Besides, there are also increased chances of iatrogenic illness due to overprescribing, poor compliance due to multiple medications, increased falls, overall poor quality of life, increased hospitalization, and even death. [44] Commonly prescribed drugs such as aspirin, warfarin, oral hypoglycemic agents, insulin, and digoxin are responsible for most hospitalizations due to adverse drug effects. The medication list should be scrutinized to see if any new signs and symptoms in the elderly are due to the prescribed medication. It is, thus, important to do a comprehensive medication reconciliation at least annually and after each transition of care to check if the medication in use is really necessary. [42] [43] Physicians can refer to the American Geriatric Society's Beers criteria which lists the potentially inappropriate medication that should be avoided in the elderly. [45]
4. Cognitive Assessment
Prevalence of mild cognitive impairment (MCI) and dementia increases with age. The prevalence of dementia is around 5% to 7%, and that of MCI is about 4 times that of dementia. [46] [47] Due to their age, multiple comorbidities, and above-described factors, older patients are at increased risk of MCI and dementia. Many of these older patients present to primary care providers with complaints of memory problems. Early detection of such conditions can help determine the reversible causes, initiate appropriate pharmacological interventions early and help patients and caregivers plan for the future. [48] Hence, providers should have a low threshold to screen for cognitive decline in elderly patients. There are various validated tools to screen for cognitive declines, such as Mini-Mental State Exam (MMSE), Montreal Cognitive Assessment (MoCA) test, and Mini-Cog. [48] [49] Mini-Cog, due to its simplicity and minimal language interpretation, can be used in multi-lingual patients. [50]
Insomnia is one of the common presenting problems of older patients. Poor sleep is associated with increased fatigue, falls, nursing home placement, poor quality of life, and overall mortality. Quality of sleep decreases with aging. Sleep disorders could be primary such as insomnia, restless leg syndrome, obstructive sleep apnea, or secondary to comorbid medical, psychiatric, behavioral, environmental, or medication side effects. Assessment of sleep disorder should include evaluation for secondary causes if any. Due to increased side-effects of hypnotics used in the treatment of insomnia, non-pharmacological interventions such as cognitive behavioral therapy, education about sleep hygiene and expected changes with aging, stimulus control, decreased daytime sleep and dietary modifications are the first line of treatment for insomnia. [51] [52]
Almost half of the cases of depression have their onset at 60 or older. Depression is associated with decreased cognition, physical and social functioning, self-care, and independence. Older patients with depression die at a higher rate; a portion of that death rate results from the highest suicide rate among older adults. [53] Options for treatment, when diagnosed early, include psychotherapy and antidepressant medications. USPSTF recommends screening for depression in all adults. [54] Patient Health Questionnaire (PHQ) 2 is a validated screening tool for depression screening, which, if positive, should be followed by PHQ 9 to diagnose depression in the elderly. [55]
- Clinical Significance
Due to the aging process, even a well-functioning older patient can deteriorate rapidly due to any 1 or a combination of issues. The development of any new signs or symptoms in the elderly can be due to the adverse effects of medication. Hence, medication reconciliation and avoidance of polypharmacy are important in every visit or each transition of care. [43] Similarly, falls are one of the major causes of disability and morbidity in the elderly. It is important to assess for falls and discuss ways to prevent them during each visit. [28] [30]
Sensory issues such as vision and hearing impairment can also lead to functional decline and masquerade as mood changes and cognitive impairment. So, patients with suspicion of such symptoms should be assessed for vision and hearing impairment. Urinary incontinence (UI), osteoporosis, and arthritis can all lead to functional decline by limiting older patients' mobility. It is important to get detailed history to diagnose the type of UI and provide appropriate treatment based on UI type. Appropriate nutrition and preventative health, use of safe medication, and surgical options like knee replacement can significantly improve the health of patients who have osteoporosis and arthritis. Early recognition of cognitive decline, including dementia, insomnia, and mood disorder, could provide an opportunity to begin behavioral and medical therapy early in the course of the disease with the possibility to reverse or at least arrest the disease progression. [48]
Older patients make the largest share of health care consumers at present. However, due to multiple issues, it can be overwhelming for providers to address all of these. The use of various standardized tools can help alleviate confusion and discrepancy in assessing older patients. It is important to address such issues on a rollover basis during each clinic visit to improve outcomes for this vulnerable population. [4]
- Other Issues
Some of the Other Issues of Concern Include
Safety assessment
- Home safety
- Driving safety
- Elder mistreatment
Goals of care and advanced directives
Safety Assessment
Home safety : About 57,000 adults above age 65 died of unintentional injuries in 2018 as per the Centers for Disease Control and Prevention (CDC), more than half of which is estimated to be due to falls. Decline in overall health at old age along with isolation leads to a higher risk of accidents at home. Clinicians should discuss common ways to prevent falls at home, such as lights, handrails, and walking assistance devices. CDC has published a checklist for home fall prevention for older adults, which can be found at https://www.cdc.gov/steadi/pdf/check_for_safety_brochure-a.pdf
Driving : Driving is a complex task and is affected by the decline in visual, motor, and cognitive ability in old age. However, it is also one of the important IADLs that help older patients maintain mobility and engage socially. Therefore, the prospect of "retiring from driving" is highly stressful for the elderly, and such recommendations should be made based on individualized assessment. Besides testing for visual acuity, neck mobility, and reaction time, a multidisciplinary approach including an ophthalmologist, a psychiatrist, a pharmacist, a physical therapist, and an occupational therapist can help assess and improve driving function. If the risk of driving is high, options for alternative forms of transportation and mobility should be discussed with patients and caregivers. [56]
Mistreatment : Elder mistreatment includes abuse and neglect. Various studies show the prevalence of elder mistreatment ranging from 2 to 36%. In the U.S., the prevalence is around 9.5%. Still, the reported prevalence is low as elder abuse tends to be underreported. [57] Some of the signs of mistreatment could be bruising in unusual places, burns, bite marks, genital trauma, pressure ulcers, BMI<17.5 kg/m2, frequent emergency room visits, etc. Such patients should be screened for mistreatment and may need further evaluation by a social worker. [58]
Goals of Care and Advanced Directives
Clinicians should discuss goals of care and advance directives primarily in ambulatory settings, well in advance of facing health crises. Effective communication allows the patient to cope with the serious illness and empowers them to direct their treatment. Goals of care discussion should be individualized as different patients would have different short or long-term goals. Similarly, advanced directives discussion allows the providers to know about the patient's wishes, prevents confusion at the end of life, and minimizes healthcare costs by deferring unwanted medical procedures. Such discussions do not increase depression, anxiety, or hopelessness in patients rather improve their quality of life and even survival by up to 25%. It also decreases stress, anxiety, and depression among family members and improves family satisfaction. [59] [60] [61]
- Enhancing Healthcare Team Outcomes
Life expectancy has improved over the last few decades due to advancements in medical science. Due to this, the population of older patients has also increased significantly. United States Census Bureau estimates around 49 million people in the US are 65 years or over in 2016. Impairment in multiple domains in the aging population inversely affects health outcomes and quality of life. Hence, a comprehensive assessment in this population is imperative for early diagnosis and treatment of a wide variety of issues in the older population. [62]
Due to the multitude of comorbidities, geriatric assessment and care require coordination between all members of the interprofessional healthcare team, including clinicians of different specialties like primary care, hospitalist, geriatrician, psychiatrist, podiatrist, dentist, to name a few, as well as nurse, social worker, and other allied health care workers such as a physical therapist, occupational therapist, nutritionist, pharmacist, psychologist, audiologist and optician. A systematic review of 29 randomized controlled trials has shown that hospitalized older patients who receive this kind of assessment have more chances of surviving and living at home than in nursing homes. [1] [Level I]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Kiran Ghimire declares no relevant financial relationships with ineligible companies.
Disclosure: Ranjan Dahal declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Ghimire K, Dahal R. Geriatric Care Special Needs Assessment. [Updated 2023 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Toward the realization of a better aged society: messages from gerontology and geriatrics. [Geriatr Gerontol Int. 2012] Review Toward the realization of a better aged society: messages from gerontology and geriatrics. Arai H, Ouchi Y, Yokode M, Ito H, Uematsu H, Eto F, Oshima S, Ota K, Saito Y, Sasaki H, et al. Geriatr Gerontol Int. 2012 Jan; 12(1):16-22.
- Forging a Frailty-Ready Healthcare System to Meet Population Ageing. [Int J Environ Res Public Healt...] Forging a Frailty-Ready Healthcare System to Meet Population Ageing. Lim WS, Wong SF, Leong I, Choo P, Pang WS. Int J Environ Res Public Health. 2017 Nov 24; 14(12). Epub 2017 Nov 24.
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. [Cochrane Database Syst Rev. 2022] Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, et al. Cochrane Database Syst Rev. 2022 Feb 1; 2(2022). Epub 2022 Feb 1.
- Toward the development of a vibrant, super-aged society: The future of medicine and society in Japan. [Geriatr Gerontol Int. 2021] Toward the development of a vibrant, super-aged society: The future of medicine and society in Japan. Iijima K, Arai H, Akishita M, Endo T, Ogasawara K, Kashihara N, Hayashi YK, Yumura W, Yokode M, Ouchi Y. Geriatr Gerontol Int. 2021 Aug; 21(8):601-613. Epub 2021 Jul 1.
- Review Geriatric oncology: a clinical approach to the older patient with cancer. [Eur J Cancer. 2003] Review Geriatric oncology: a clinical approach to the older patient with cancer. Repetto L, Venturino A, Fratino L, Serraino D, Troisi G, Gianni W, Pietropaolo M. Eur J Cancer. 2003 May; 39(7):870-80.
Recent Activity
- Geriatric Care Special Needs Assessment - StatPearls Geriatric Care Special Needs Assessment - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- NLN Credentialing
- Assessment Services
- CNEA Accreditation
- NLN Foundation
- Mission & Core Values
- History & Archives
- Board of Governors
- Senior Management
- Consultants & Speakers Bureau
- NLN Nominations
- Career Center

- Aging with a Disability
Assessment of a Person with Disability Checklist
- Brief Historical View of Disability and Related Legislation
- Communicating with People with Disabilities
- Definitions Related to Disability
- Guide for Integrating Standardized Patients with Disabilities in Nursing Curriculum
- Guide for Integrating Standardized/ Simulated Patients with Intellectual and Developmental Disability in Nursing Curriculum
- Overview and Introduction to Disability
- Pregnancy in Women with Disabilities
- Inclusion of Disability in Nursing Education: Rationale and Guidelines
Assessment of a Patient with a Disability © Checklist
Download the PDF checklist
Needed for Effective Assessments Effective communication and interpersonal skills are essential in conducting any patient assessment; this includes making eye contact with the interviewee and being at the patient’s eye level. This requires sitting down to ensure that you are at the patient’s eye level and do not require the patient to look up to communicate with you if he or she in in a wheelchair or sitting in a chair or on a motorized scooter. Patient to be Assessed : Ms. Kathryn H., a 60-year-old woman, comes to the outpatient clinic for an appointment with a primary health care provider. She is accompanied by her grown daughter. She has not been seen by a health care provider for over a year and a half. This is your first encounter with Ms. H. and you are assigned to obtain information about her and the reason for her health care visit. Overview of Assessment: 1)_____Identify disability as identified by the patient. (It is essential to address the patient’s disability in the health history and physical assessment You will not upset the patient by asking about a disability; the patient is usually very aware of the disability and very knowledgeable about it, and likely will be distressed if you don’t consider the disability when you obtain a health history and complete a physical assessment. Examples of questions or probes to use to ask about patient’s disability: “Would it be okay if I ask you a few questions about your disability?” and “Please tell me about your disability.”) When you enter the room, you note that Ms. H. is sitting in a chair. She looks comfortable and not in any acute distress. Along side her is a motorized scooter. After introducing yourself, verifying the patient’s name with her and asking Ms. H. the purpose of the visit, it is appropriate to comment on the scooter: “Ms. H., can you tell me why you use the motorized scooter?” She responds, “I use it to get around when I am out of my house. I have used it for about three years.” Because she has not reported why she is using the scooter, it is appropriate to ask: “Do you use it because of fatigue, issues walking, or another reason?” She replies, “I use it because of weakness of my legs and because I fall easily.” Your next response could be: “Can you tell me the cause of your muscle weakness and falls?” or “Do you have an underlying disability that causes your muscle weakness?” In response to this question, Ms. H. responds: “I had polio when I was four years old. I did okay over the years, but when I hit about 50 years of age, I started noticing muscle weakness and I started to stumble a bit. I was diagnosed about six years ago with post-polio syndrome. The muscle weakness has increased and I have foot drop. So I wear splints on both lower legs.” 2) _____Assess patient's ability to communicate and participate in health history and physical assessment. (Assume that the patient is able to participate in discussion and conversation rather than assuming that he or she is unable to do so because of the disability. Communicate directly with the person with a disability rather than to a family member or caregiver who is with the patient.) Although Ms. H.’s daughter is with her, it is essential to discuss her disability with Ms. H. rather than to direct questions to her daughter. Since Ms. H. will be asked about her full health history and have a physical examination, it would be appropriate to ask if she has limitations that affect other parts of her body other than her lower extremities. “Ms. H., does the post-polio syndrome or other health problem affect other parts of your body in addition to your legs?” In response to that question she replies: “I have some weakness of my arms, too, but that is not as big a problem as the weakness of my legs.” 3) _____Identify accommodations and modifications (e.g., signing, large print, other, etc.) needed by person with a disability to participate in the health history and assessment. (Determine what assistance is needed to transfer the patient safely from a wheelchair to an exam table so that a complete assessment, including pelvic or testicular and rectal exam, can be conducted if indicated. Arrange for an interpreter if needed [it is not appropriate for a patient’s family member or other accompanying person to serve as interpreter].) In preparation for the physical exam that will be conducted by the nurse practitioner, it would be appropriate to ask Ms. H. if she needs assistance in transferring from the chair to the examination table when it is time for her to do so. “How can I help you get on the exam table safely? Do you need assistance removing your coat and putting on a gown?” 4) _____Include all aspects of health history and physical assessment that would be included for all patients. (The health history and physical assessment should address the same issues that would be addressed with a person without a disability. For example, the health history should include sexuality, sexual function, reproductive health issues, preventive health care practices, and lifestyle behaviors. Assume that a person with a disability participates in the same activities and behaviors as those without a disability.) When obtaining the health history and conducting the physical assessment, it is important to ask the same questions you would ask of any other patient. “Ms. H., do you exercise regularly? What kind of exercise do you do? How often do you exercise? When was your last GYN exam? When did you have your last mammogram? Were you able to stand for the mammogram? Have you had a colonoscopy? Have you ever had a DEXA to assess your bone density? Are you sexually active?” 5) _____Use “person-first language” in interactions with and about persons with disabilities. (Although some disability groups [e.g., the Deaf community] prefer to be identified by their disability [“the Deaf person”], most prefer NOT to be identified by their disability. Language that refers to the person first [“person with a disability”] rather than their disability is more acceptable.) When referring to Ms. H. to other health care providers or staff, it is important to refer to her as “a woman with a disability (or post-polio syndrome) rather than as a “disabled woman.” If you refer to other individuals with disabilities when communicating with Ms. H., it is also important to use person-first language rather than refer to them as “the disabled” or “disabled people.” “Some women with disabilities have difficulty standing to have a mammogram or standing for the time it takes to have it done. Do you have difficulty doing so?” Disability-specific Issues 1) _____Assess the effect of a patient’s disability on his/her ability to obtain health care. (Assessment should address the interaction of person’s disability and health care, his or her ability to manage self-care activities, follow health care recommendations, and obtain preventive health screening and follow-up care.) Many individuals with disabilities do not receive health care as often as is recommended because of transportation issues and other barriers, including failure of clinical facilities and staff to provide accommodations that enable them to participate in health care and screening, so it is important to ask about those issues. “Ms. H., has your disability (or post-polio syndrome) made it difficult to obtain required health care, such as GYN exams, mammography, or other screening or care? How has it limited your ability to receive care?” 2)______Assess patient for abuse or risk for abuse (physical, emotional, financial, and sexual) by others (family, paid care providers, strangers). (Questions should be asked privately when no one else, including family and care providers, is in the room or able to overhear the conversation. Questions specific to abuse of persons with disability include: Have they been prevented from using wheelchair, cane, respirator, or other assistive device; have they been refused help for important personal needs [taking medications, getting to bathroom, getting out of bed, getting dressed, getting food or drink]. If abuse is detected, assess patient’s access to accessible information, resources, shelters, and hotlines.) After asking her daughter to leave the room for a few minutes, it is appropriate to ask Ms. H. if she has experienced any abuse or personal violence. Asking specific questions related to her disability may uncover issues that don’t affect individuals without disabilities. “Ms. H., do you feel safe? Have you ever had any concerns about your safety? Has anyone prevented you from using your scooter or other assistive devices? Has anyone prevented you from receiving the help or care you need?” 3)_____Assess the patient for risk of falls. (Ask about previous falls and injuries due to falls. Ask about impaired balance, muscle weakness, changes in gait, changes in vision, confusion. Ask if assistive devices are available and used to prevent falls.) Ms. H. has already indicated that she falls easily. So questions about her risk for falls are very relevant and appropriate. “Ms. H., can you tell me when (or in what situations) you are likely to fall? Tell me about the times you have fallen and any injuries you have had as a result of a fall. Do you have strategies to reduce your risk for falling and sustaining injury from falling?” 4)______Assess patient for depression. (Do not assume that depression is “normal” because a person has a disability. If a person with a disability has depression, treatment should be offered just as any other patient would have treatment offered.) It is appropriate to ask Ms. H. if she has experienced bouts of depression and important to recognize that having depression is not a “normal” reaction to having a disability. Further, individuals with disabilities who are depressed should be evaluated and appropriate treatment for depression should be provided. “Ms. H., do you ever experience depression? Do you have days when your mood keeps you from wanting to get out of bed or leave the house or your room? Have you ever been treated for depression?” 5) _____Assess patient for secondary conditions or risk for secondary conditions. (Secondary conditions are those conditions that result from having a disability or result from treatment of a disability [e.g., pressure ulcers, injuries]. Identify barriers to health care that may increase risk of secondary conditions [e.g., lack of transportation, non-participation in health promotion activities].) Ms. H. has already indicated that she falls easily, increasing the risk for falls-related injuries. It is important to determine if she is at risk for other secondary conditions, such as pressure ulcers and other health problems that may be related to transportation barriers or non-participation in health promotion activities, such as lack of exercise (weight gain, increased cardiovascular risks). “Tell me about any injuries that you have experienced as a result of falling. What strategies have you used to reduce your risk for falling? What strategies do you use to reduce the risk of injury when you do fall?” “Are you able to get around for appointments and to meet your day-to-day needs? Does anything hold you back from being able to do things you would like to do?” 6) _____Assess what accommodations the patient has made at home or needs at home to encourage or permit self-care and independence. Identify accommodations needed during hospital stay or when out of the home. (Accommodations may range from use of assistive devices or simple rearrangement of the home to structural modifications that enable the person with a disability to remain in the home and to participate safely in his or her preferred setting. Home care nurses and therapists [occupational or physical therapists] can be helpful in assessing the home environment and suggesting modifications that would increase the ability of individuals with a disability to function safely in their own home. Determine if patient has or requires a bladder or bowel management program, uses alternative approaches to eating and drinking fluids, or has had a procedure to make management of bowel, bladder, and nutrition possible [e.g., self-catheterization, urinary diversion, insertion of PEG tube, etc.). “In addition to the motorized scooter that you use when outside your home, what assistive devices or accommodations do you use in your home, such as walker, cane, or crutches? Have you ever fallen when using your assistive devices, or when not using the devices or when transferring from the scooter? Do you believe that you use the devices safely? Do you have a need for other modifications or accommodations that would make it easier for you at home or when out of your home? Are you interested in having an evaluation by an occupational or physical therapist to meet with you or visit you at home to determine if other devices or accommodations might be helpful to you?” 7) ____Determine what preparation and accommodations are needed during hospital stays, emergency room or clinic visits, acute illness or injury, and other health care encounters to enable a patient with disability to be as independent as he or she prefers. (Determine if facility staff are informed about the activities of daily living for which the patient will require assistance. Determine if accommodations are in place and readily available to enable the patient to use his or her assistive devices (hearing/visual aids, prostheses, limb support devices, ventilators, service animals). Determine what plans or strategies are in place to ensure minimize consequences of immobility because of surgery, illness, injury, or treatments.) “Ms. H, in order to provide the best care for you while you are in the hospital, please tell me what type of assistance you need to transfer from the chair or scooter to the exam table (or from the bed to a chair). Is there any special way to provide this assistance so that we meet your need for comfort and safety? Other than your scooter, do you use any other assistive devices at home that would help you while in the hospital?” 8)____Assess what accommodations and alternative formats of instructional materials (large print, Braille, visual materials, audiotapes, interpreter) are needed by the patient with a disability. (Determine if patient instruction materials are consistent with modifications [e.g., use of assistive devices] needed by the patient with disabilities to enable him or her to adhere to recommendations. Determine if the modifications made in educational strategies address learning needs, cognitive changes, and communication impairment.) Ms. H. wears glasses, but indicates that no other accommodations or alternative formats are needed for her to read and understand instructional materials. If she were hard of hearing or had significant visual impairment, alternative methods of providing educational information and instructions must be provided. 9) ____Assess engagement of patient with disabilities in health promotion strategies and the patient’s awareness of their potential benefits (e.g., improved quality of life, prevention of secondary conditions). (Assess patient’s awareness of accessible community-based facilities [e.g., health care facilities, imaging centers, public exercise settings, transportation] to enable them to participate in health promotion.) It would be important to ask Ms. H. about her knowledge or awareness of places where she can go for exercise or preventive screening that are accessible and can accommodate her. “If you wanted to go to a gym or fitness center, is there one near your home that is accessible? Are the centers to have preventive screening accessible to you? Do the staff provide assistance to enable you to have screening done?”
Author Information
Suzanne C. Smeltzer, EdD, RN, ANEF, FAAN Professor Emerita and Research Professor
Bette Mariani, PhD, RN, ANEF, FAAN Vice Dean for Academic Affairs and Professor
Colleen Meakim, MSN, RN, CHSE-A, ANEF Director, Second Degree Track
M. Louise Fitzpatrick College of Nursing, Villanova University
© Suzanne C. Smeltzer, EdD, RN, ANEF, FAAN; Bette Mariani, PhD, RN, ANEF, FAAN; Colleen Meakim, MSN, RN, CHSE-A, ANEF; M. Louise Fitzpatrick College of Nursing, Villanova University, 2017.
Users are asked to cite the source for these Villanova University developed resources as developed by the Villanova University College of Nursing and retrieved on the NLN website.
Geriatric Care Special Needs Assessment
Affiliations.
- 1 Texas Tech University Health Science Center El Paso
- 2 Texas Tech University Health Sciences Center, El Paso, TX
- PMID: 34033334
- Bookshelf ID: NBK570572
The elderly population (age >65 years) is increasing throughout the world, leading to increased hospitalization. There was a 16.7% increase in elderly hospitalization from 2003-2009 in the United States. This rising hospitalization has impacted healthcare services delivery. With the aging population comes a multitude of chronic conditions. It is estimated that 9 out of 10 Americans have at least one chronic condition by age 80.
Due to multiple comorbidities and frailty, the elderly are at increased risk of adverse outcomes with each clinical insult. Besides the common comorbidities such as diabetes and hypertension, older patients can present with atypical presentation too. For example, a patient with sepsis may present without fever, or a patient with Urinary Tract Infection (UTI) may present with confusion. The elderly population varies in cognitive, physical, and social functioning and thus requires different levels of care based on individual needs and functional status.
Geriatric assessment, thus, includes a coordinated approach for the physical, functional, and psychosocial assessment of the elderly and formulate an integrated plan of care.
Copyright © 2024, StatPearls Publishing LLC.
- Continuing Education Activity
- Introduction
- Issues of Concern
- Clinical Significance
- Other Issues
- Enhancing Healthcare Team Outcomes
- Review Questions
Publication types
- Study Guide

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
17 Assessment of Special Populations
Learning objectives.
At the end of this chapter, the learner will:
- Identify age-related variations in conducting a health assessment.
- Discuss the involvement of caregivers/guardians in the assessment process.
- Complete the Activity of Daily Living Assessment for geriatric patients.
- Discuss abuse and neglect for at-risk populations.
I. Overview of the Special Populations
In prior chapters, the essential knowledge of health assessment was laid out to prepare the nurse to assess adult patients in a clinical setting. Information on comprehensive assessment and focused assessments were also presented, with the aim of preparing the nurse to use clinical reasoning to choose the appropriate assessment for each clinical situation presented. Examples of special populations include obstetric examination during pregnancy, labor and delivery, and the postpartum period, newborn assessment, pediatric assessment, and geriatric assessment. This chapter will demonstrate how the health assessment is adapted for the pediatric and geriatric populations.
Growth and Development
Growth and development is an ongoing process that begins at conception and continues through the remainder of our lives. There is a broad spectrum of physical and psychological changes that are part of the maturation and life of the individual.
Growth is a physical change that can be weighed and measured. Development is psychological and social changes to the individual such as behaviors and thinking patterns. Growth and development are two complementary processes that together make up the individual.
The rate of development and growth is dependent on many factors such as age and genetic disposition…
The newborn’s specific assessment findings:
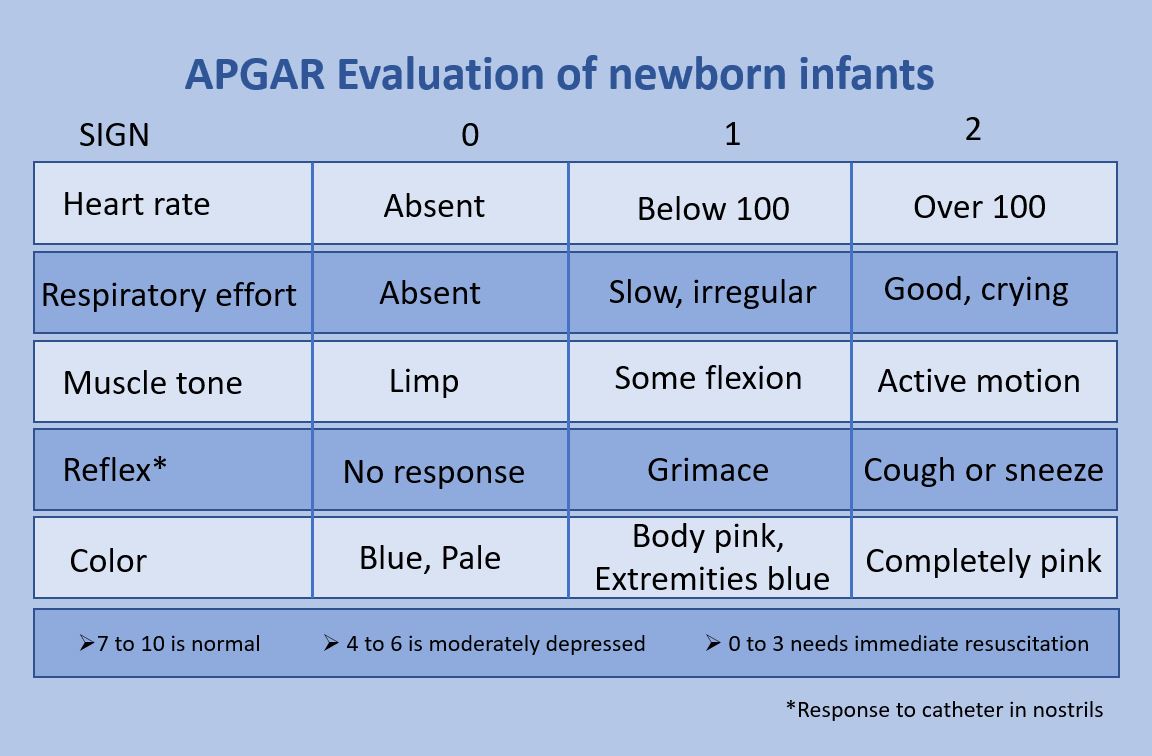
The chart above is the work of Dr. Vijaya Chandar:https://commons.wikimedia.org/wiki/Category:Apgar_score#/media/File:APGAR_score.jpg
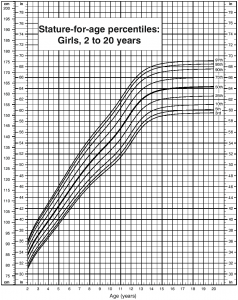
Some of the main assessment tools used to assess children are the Milestone and growth charts. Developmental Milestones are used to help ensure that each child is behaving and appropriate growth is occurring intellectually, cognitively, emotionally, and socially. The growth in all capacities is influenced by culture, social norms, and institutions in the child and family’s life. Growth charts are used to assess how well a child is growing and how that growth compares to other children in the country.
Assessment findings of the newborn include assessing different body systems. See below:
- A newborn’s skin is grayish to dusky blue in color until the baby starts breathing at which time the baby’s skin will return to the appropriate color and tone. The baby is also wet, covered in streaks of blood, and coated with a white substance known as vernix caseosa. The newborn may also have Mongolian spots, birthmarks, or peeling skin, particularly at the wrists, hands, ankles, and feet.
- The newborn’s body dimensions include narrow shoulders and hips, a slightly protruding abdomen, and relatively short upper and lower extremities.
- The baby will weigh between 5-10 pounds and measure between 14-20 inches (35.6-50.8 cm)
- The head is large in the proportion to the rest of the body and the cranium is large compared to the rest of the face., and the fontanels will still be open. The head may also be misshapen from coming through the birth canal this will resolve within days or weeks.
- The skin may be covered with lanugo, a fine downy body hair for a few weeks.
- The newborn’s genitals are swollen and reddened, with male infants having an unusually large scrotum.
- All babies will have enlarged breasts with possible milk secretions that range from clear to milky to bloody. These findings are due to the mother’s hormones.
- The umbilical cord will dry and fall off in 3 weeks.
Below are links to Growth charts from 0-24 months for male and female children from the Center for Disease Control and Prevention: https://www.cdc.gov/growthcharts/who_charts.htm
Growth Charts for girls 0-24 months
Growth Charts for boys 0-24 months
Here is an example. Many items are measured this way to ensure that children meet wellness goals. Items include height, length, weight, and in babies head and chest circumference. Growth charts were noted until age 12.
Milestones: The first year of life is a year of rapid growth and body changes/functions. the nurse will assess the patient according to developmental stages. The first stage would be 0 months-1 year. Toddlers 1-3 years, Pre-Schoolers 3-6, School ager 6-12-year-old also called middle childhood, 12-18-year-old Adolescence.
The 5-year-old child old realizes what is real and what is not, is aware of gender, and starts to create a social group, grows in independence, speaks clearly, and has improved balance and activity tolerance. The five-year-old is in or getting ready for pre-school.
The twelve-year-old child has hobbies, dexterity, becomes independent with Activities of Daily Living, can tell time, understands complex commands, and enjoys using the telephone, plays with friends of the same gender, and by 10 years old starts playing with the other sex, enjoys talking to others. See the link below for further details: https://www.stanfordchildrens.org/en/topic/default?id=the-growing-child-school-age-6-to-12-years-90-P02278
The 12-18-year-old-Adolescents rapid growth with changes to the body’s composition, height, and weight. Sexual maturity occurs. Changes also occur to the respiratory and cardiac systems. There is improved ability to think including improvement to attention span, memory, processing speed, organization, and Metacognition. Metacognition is necessary for social cognition and results in increased introspection, self-consciousness, and intellectualization. Risk-taking behavior occurs because of continued brain development especially the frontal lobe. There is rapid cognitive growth also that interacts with experience, knowledge, and social demands.
Please use this link to review the milestones that are expected and guide the assessment in children 1 month to 6 years. https://depts.washington.edu/dbpeds/Screening%20Tools/Devt%20Milestones%20Table%20(B-6y)%20PIR%20(Jan2016).msg.pdf
Please use this link to review the milestones that are expected and guide the assessment in children 6-12 years old. https://www.stanfordchildrens.org/en/topic/default?id=the-growing-child-school-age-6-to-12-years-90-P02278
Please use this link to review the milestones that are expected and guide the assessment in Adolescents. https://courses.lumenlearning.com/boundless-psychology/chapter/adolescence/
Now that the milestones and growth charts have been discussed please review the video below which presents a comprehensive approach to the assessment of children:
Geriatric Assessment:
Geriatrics refers to the medical care of older adults which normally refers to adults over 65 years old. Aging is the irreversible, inevitable decline in organ function (Merck Manual). The decline is gradual and occurs over a period of time. The speed of aging is determined through genetics, environmental and other factors. This decline will occur even if the patient is healthy. Illness, environmental risks, or poor lifestyle choices may speed up aging. The body systems that age first and profoundly affect homeostasis are the cardiovascular, renal, and central nervous. Therefore, when assessing these systems take the time to be thorough even if the patient seems healthy as initially the baseline function of these organs will not be affected. Please click on this link to review the Physiological Age-related changes Selected Physiologic Age-Related Changes
When diseases interact with the normal decline in organ function geriatric-specific complications, now called geriatric syndromes, occur. An example would be an older adult having undiagnosed Pneumonia and the first manifestation of pneumonia is delirium. This presentation is because of the decline in organ function. Whereby minor illnesses are paired with unusual and unlikely signs of illness. Aging organs are also more susceptible to injury; eg, intracranial hemorrhage is more common and is triggered by less clinically important injury in older adults. Other life-changing medical diagnoses like a Cerebral Vascular Accident occur with minimal injury. The nurse should also monitor the older adult closely for debilitating diseases like Alzheimer’s disease and Atrial fibrillation.
Assessment of the older adult will need more time and attention, especially for the very old or frail patients. Obtaining needed information from a health history and the physical exam itself may need to occur on two separate occasions because of fatigue. The second reason for needing more time to complete the assessment is that many older adults have either or both an increased number of health care disorders or increased complexity in the diagnosed disorders. The third reason for added time is to ensure that polypharmacy does not occur. Please click on the link to review the medications that older adults should not be taking, Potentially Inappropriate Drugs in Older Adults
The Healthcare team’s duty is to address and maintain patient function, prevent falls, and improve the quality of health, encourage exercise and healthy eating, and give the older adults a voice in their care. The geriatric assessment has four components:
Functional ability: Ability to do activities of daily living (ADLs) and instrumental ADLs (IADLs) are assessed. ADLs include eating, dressing, bathing, transferring between the bed and a chair, using the toilet, and controlling bladder and bowel. IADLs enable people to live independently and include preparing meals, doing housework, taking drugs, going on errands, managing finances, and using a telephone (Merck Manual).
Physical Assessment: This section will be different as it should have a problem-based approach that addresses both current and possible future medical disorders/diseases including problems with vision, hearing, ambulation-gait, balance, and incontinence.
Cognition and mental health: Several validated screening tests for cognitive dysfunction (eg, mental status examination ) and for depression (eg, Geriatric Depression Scale , Hamilton Depression Scale) can be used. (Merck Manual)
Socio-environmental situation: The nurse should assess the patient’s: social support system, the utilization of services that will enable hobbies, living independently, and being a satisfied member of a community. Services should address any disabilities, special needs, or home safety, and may need social work involved in the plan of care.
- Do you have difficulty performing functional tasks and need if assistance is needed how much? An example of a functional task is getting out of a chair without using the arms.
- Have you ever fallen and if so how many times? How has the fall affected your self-esteem, independence, mobility, and socialization?
- Do you have urinary and/or fecal incontinence? If yes what have you done to manage the condition> Have you spoken to your primary care provider about the incontinence? What appliance are you using? Can you afford the appliances?
- Do you have any Pain? Where is it located and how long have you had it? How is the pain managed at home?
- What sources of social support, particularly family or friends do you have? How often do you see them? How far away do they live? What interactions or activities are completed together.
- Depressive symptoms- Use the tools provided by the facility and linked above.
- Vision or hearing difficulties, Have you been prescribed glasses or a hearing aid? Are you using glasses or a hearing aid. If yes how are they cleaned? if no then why? Is the vision or hearing loss affecting your functioning or activity of daily living?
- Whether the patient has specified a ‘lasting power of attorney for healthcare. If there is a power of attorney then does the power of attorney know and respect your wishes.
- Below is a video example of a Geriatric assessment:
Geriatric Head to Toe and Functional Assessment by the Multi-disciplinary team. Please click the link if the video is not visible.https://youtu.be/-eHPugoC5sE
https://youtu.be/-eHPugoC5sE
Geriatric Head to Toe and Functional Assessment by the nurse. Please click the link if the video is not visible:https://youtu.be/s7LSCrGWCys
Knowledge check
II. Anatomy and Physiology
Click the link below to review how the anatomy and physiology of the baby, toddler, school-age child, and adolescent differs from an adult. In the assessment process, you will need to apply your knowledge of how age changes both the landmarks used to assess a patient and what are considered normal findings/values.
Physiology from birth through death
III. Medical Terminology
IV. Step by Step Assessment
- Perform hand hygiene.
- Check room for contact precautions.
- Introduce yourself to the patient.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient.
- Assemble equipment prior to starting the exam.
- Be organized and systematic in your assessment.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure patient’s privacy and dignity.
- Apply principles of asepsis and safety.
- Use age-appropriate methods to Check Vital Signs.
V. Documentation of Assessment Findings
Please click the link below to see a sample of the narrative documentation for a Head-to-Toe assessment related to an older adult:
https://www.opennotes.org/tools-resources/for-patients/reading-your-notes/
A sample Note
VI. Related Laboratory and Diagnostic Findings
Blood tests related to the pediatric patient at an outpatient wellness visit will include a complete blood count with differential and possibly a metabolic panel to review electrolytes. The need for further blood and radiology testing will be driven by patient history, current symptoms, signs, and assessment findings. Testing for iron deficiency or vitamin deficiency, diabetes and HIV, and other STDs can be seen in both the pediatric and geriatric populations. Older adults will be tested for cholesterol and triglycerides periodically if at risk for heart disease. Calcium and Vitamin D levels will be checked in older adults if at risk for Osteoporosis.
Some of the commonly ordered radiological tests include the Chest X-ray when the following medical diagnoses are suspected: Asthma, Pneumonia and CardiacMyopathy. X-rays of the arms and legs will be ordered for pediatric patients from fall-related to outdoor activity, sports, or child abuse. In the older adult again, these X-rays are ordered for falls that occur in or out of the home because of sarcopenia, lack of balance, or inactivity which too leads to muscle mass loss.
Cat Scans are used for many reasons including head injuries. In the pediatric setting these injuries are trauma bases and in the geriatric population trauma is one reason but the next reason will be Cerebral Vascular Accidents.
Myocardial Infarctions (MI) are the main cause of death for older adults and as such catherization of the clogged vessel is imperative as soon as possible with an admitting EKG and chest X-ray.
Type your key takeaways here.
VII. Learning Exercises
Knowledge check: Please complete the following activities.
VIII. Attributions and References
- Human Physiology/Development: birth through death https://en.wikibooks.org/wiki/Human_Physiology/Development:_birth_through_death
- Common Terms Related to Aging https://courses.lumenlearning.com/atd-herkimer-biologyofaging/chapter/common-terms-related-to-aging/
- Child Developmental Stages-Why is it Important? https://open.maricopa.edu/devpsych/chapter/chapter-4-infancy-and-toddlerhood/#:~:text=For%20each%20milestone%2C%20there%20is,weeks%20and%204%20months%20old
- Apgar score https://simple.wikipedia.org/wiki/Apgar_score
- Define Fontanels https://courses.lumenlearning.com/ap1/chapter/embryonic-development-of-the-axial-skeleton/
- Growth Chart https://pediasure.com/child-development-nutrition/average-height-weight-kids?gclid=CjwKCAjwlYCHBhAQEiwA4K21m3X3pjjcG4oIgsLkDsljtXeBX3CfzVkJ-F44lg82ut-hTrV5vKyuoBoCC4wQAvD_BwE&gclsrc=aw.ds
- Boundless Psychology Adolescence Physical Development in Adolescence https://courses.lumenlearning.com/boundless-psychology/chapter/adolescence/
- Rojas, Y., Children’s Health Care October 5, 2018 https://www.chcmass.com/2018/10/05/the-stages-of-child-development/
- Important Milestones: Your child by five years old. CDC https://www.cdc.gov/ncbddd/actearly/milestones/milestones-5yr.html
- The Growing Child: School-Age (6 to 12 Years) Standford Children’s Health Lucile Packard Children’s Hospital Standford https://www.stanfordchildrens.org/en/topic/default?id=the-growing-child-school-age-6-to-12-years-90-P02278
- Human Growth and Development https://www.encyclopedia.com/medicine/encyclopedias-almanacs-transcripts-and-maps/human-growth-and-development-0
- Common Terms related to Aging https://courses.lumenlearning.com/atd-herkimer-biologyofaging/chapter/common-terms-related-to-aging/
- Geriatric examination (head to toe complete assessment of old patient)OSCE https://youtu.be/s7LSCrGWCys
- 2.3 Components of a health history https://wtcs.pressbooks.pub/nursingskills/chapter/2-3-components-of-a-health-history/
- Health History https://opentextbc.ca/clinicalskills/chapter/2-4-health-history-subjective-assessment/
- Adult health history form https://docs.google.com/document/d/1cw1THqBpHKi7_IggH3FoiVy3HidVzoO1dWpzupkLL1M/edit
- Review of body systems https://wtcs.pressbooks.pub/nursingskills/chapter/2-9-review-of-body-systems/
- 2.8 FUNCTIONAL HEALTH AND ACTIVITIES OF DAILY LIVING https://wtcs.pressbooks.pub/nursingskills/chapter/2-8-functional-health-and-activities-of-daily-living/
- Joint Pian in Children https://www.columbiadoctors.org/childrens-health/pediatric-specialties/rheumatology/treatments-conditions/joint-pain-children
- Perinatal outcomes from preterm and early term births in a multicenter cohort of low risk nulliparous women https://www.nature.com/articles/s41598-020-65022-z
- Child abuse in the US: Resouces for journalists https://journalistsresource.org/health/child-abuse-incidence-risk-factors-sentencing/
- Child abuse https://www.mayoclinic.org/diseases-conditions/child-abuse/symptoms-causes/syc-20370864
- Elder Abuse: What research says about prevalence, assessment and prevention https://journalistsresource.org/politics-and-government/elder-abuse-research-prevalence/
- Introduction to Geriatrics Merck Manual https://www.merckmanuals.com/professional/geriatrics/approach-to-the-geriatric-patient/introduction-to-geriatrics
- Evaluation of the older adult Merck Manual https://www.merckmanuals.com/professional/geriatrics/approach-to-the-geriatric-patient/evaluation-of-the-older-adult#v1132000
- Spirgiene, L., and Brent.L.Fragility Fracture Nursing: Holistic Care and Management of the Orthogeriatric Patient [Internet]Chapter 4 Comprehensive Geriatric Assessment form a Nursing Perspective. June 16, 2016. Retrieved 14:38 July 30, 2021. https://www.ncbi.nlm.nih.gov/books/NBK543827/
Health Assessment Guide for Nurses Copyright © by Ching-Chuen Feng; Michelle Agostini; and Raquel Bertiz is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.

Share This Book
- (872) 216-6658
- [email protected]

A Non Profit Organization
If you have questions related to training on our TCOM tools or the TCOM Training site, please reach out to [email protected] . All other questions can be sent to [email protected] . You can also visit us at the IPH Center at iph.uky.edu
Stay updated on all the latest TCOM content.
From upcoming podcasts to video series and conferences, we’ve got you covered.
THE ADULT NEEDS AND STRENGTHS ASSESSMENT (ANSA)
WHAT IS ANSA?
The ANSA is an open domain tool that is free for anyone to use. There is a community of people who use the ANSA and share experiences and additional items and supplementary tools.

a. No evidence b. Watchful waiting/prevention c. Action d. Immediate/Intensive Action
FOR STRENGTHS:
1.Centerpiece strength 2. Strength that you can use in planning 3. Identified-strength-must be built 4. No strength identified
The Adult Needs and Strengths Assessment (ANSA) is a multi-purpose tool developed for adult’s behavioral health services to support decision making, including level of care and service planning, to facilitate quality improvement initiatives, and to allow for the monitoring of outcomes of services.
The ANSA is currently used in a number of states and Canada in applications hospitals, emergency departments, psychosocial rehabilitation programs, and ACT programs. The ANSA was developed from a communication perspective so as to facilitate the linkage between the assessment process and the design of individualized service plans including the application of evidence-based practices.
The ANSA was developed from a communication perspective so as to facilitate the linkage between the assessment process and the design of individualized service plans including the application of evidence-based practices. The original version, the Severity of Psychiatric Illness (SPI), was created in the 1990’s to study decision-making in psychiatric emergency systems. The ANSA expands on the concepts of the SPI to include a broader description of functioning and include strengths with a recovery focus.
The ANSA is easy to learn and is well liked by recipients, family members, providers and other partners in the services system because it is easy to understand and does not necessarily require scoring in order to be meaningful to an individual and his/her family. The way the ANSA works is that each item suggests different pathways for service planning. There are four levels of each item with anchored definitions; however, these definitions are designed to translate into the following action levels (separate for needs and strengths)
In terms of quality improvement activities, a number of settings have utilized a fidelity model approach to look at service/treatment/action planning based on the ANSA assessment. A rating of ‘2’ or ‘3’ on a CANS needs suggests that this area must be addressed in the plan. A rating of a ‘0’ or ‘1’ identifies a strength that can be used for strength-based planning and a ‘2’ or ‘3’ a strength that should be the focus on strength-building activities.
Finally, the ANSA can be used to monitor outcomes. This can be accomplished in two ways. First, items that are initially rated a ‘2’ or ‘3’ are monitored over time to determine the percent of youth who move to a rating of ‘0’ or ‘1’ (resolved need, built strength). Or, dimension scores can be generated by summing items within each of the dimensions (Problems, Risk Behaviors, Functioning, etc). These scores can be compared over the course of treatment. ANSA dimension scores have been shown to be valid outcome measures in hospital, partial hospital, psychosocial rehabilitation, and intensive community services.
The ANSA has demonstrated reliability and validity. With training, any one with a bachelor’s degree can learn to complete the tool reliably, although some applications require a higher degree. The average reliability of the ANSA is 0.75 with vignettes, 0.86 with case records, and can be above 0.90 with live cases. The ANSA is auditable and audit reliabilities demonstrate that the ANSA is reliable at the item level. Validity is demonstrated with the ANSA relationship to level of care decisions and other similar measures of symptoms, risk behaviors, and functioning.
ANSA DOWLOADS
Standard ANSA Manuals
Standard ANSA Forms
TCOM Training Support Info
Phone : 872-216-6658
Email : [email protected]
*Responses could take up to 1 business day depending on volume
Our Location
Praed Foundation
550 N Kingsbury St, Apt 101, Chicago IL 60654
General Inquiries: [email protected]
2023 © All rights reserved
Made with ❤ by handcutdesigns.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Chapter 13: Special Populations in Ambulatory Care
Stacey Hobbick
Learning Objectives
By the end of this chapter, the learner should be able to:
- Define and identify special populations in the context of ambulatory care.
- Recognize the unique needs and challenges of special populations.
- Apply comprehensive assessment techniques tailored to each special population.
- Describe the legal and ethical considerations in treating special populations.
Introduction to Chapter 13
Special populations in the context of ambulatory care encompass various groups of individuals who require unique considerations and tailored healthcare approaches. These populations may include the elderly, children, pregnant women, individuals with disabilities, those with chronic diseases, and others whose care might need particular attention and strategies. The concept goes beyond merely identifying these groups; it involves recognizing their specific needs, preferences, potential barriers to care, and aligning healthcare practices accordingly.
Understanding and catering to special populations is of paramount importance in ambulatory care. The ability to recognize the unique needs of these individuals and groups not only ensures equitable access to healthcare services but also significantly enhances the quality of care delivered. In an increasingly diverse society, healthcare professionals must be equipped with the knowledge and tools necessary to provide compassionate and competent care to all patients, irrespective of their specific needs or backgrounds. By focusing on special populations, healthcare providers can create more tailored and effective care plans, fostering better health outcomes and patient satisfaction.
Through this chapter, we delve into the intricate aspects of caring for special populations in ambulatory settings, addressing the necessary theoretical underpinnings, practical applications, ethical considerations, and the latest technological advancements. Whether you are a seasoned practitioner or a student beginning your nursing journey, this information provides a vital foundation for excellence in patient-centered care for those who need it the most.
Chapter 13 Key Terms
Special Populations: Groups of individuals who require specific attention, tailored approaches, and specialized care plans within a healthcare setting, such as the elderly, children, pregnant women, individuals with disabilities, and chronic disease patients.
Comprehensive Assessment: A thorough and detailed evaluation of a patient’s health, encompassing physical, mental, emotional, and social aspects. For special populations, this includes additional evaluations related to age, disability, chronic conditions, cultural background, or other factors specific to the population.
Tailored Care Plans: Individualized care strategies developed for a patient, considering their unique needs, preferences, and characteristics. In the context of special populations, these plans are particularly sensitive to the specific requirements of each group.
Cultural Sensitivity: The awareness, understanding, and respect of cultural differences, including beliefs, practices, and values, in healthcare provision. This concept is crucial in the treatment of diverse special populations to ensure equitable and respectful care.
Telemedicine: The use of technology to provide clinical health care from a distance, often used to enhance the accessibility and efficiency of care for special populations.
Patient Rights: The legal entitlements and ethical guidelines related to the treatment of patients, including confidentiality, informed consent, and autonomy. Special attention to these rights is necessary when treating special populations.
Adaptive Equipment: Tools and devices modified or specially designed to assist individuals with disabilities or other special needs. These play a vital role in enhancing the independence and quality of life for special populations in ambulatory care
13.1 Identification of Special Populations
The recognition and understanding of special populations within ambulatory care require a thoughtful examination of various groups that may require unique considerations.
Among the elderly population, age-related changes and challenges come to the fore. These may include physical impairments, cognitive decline, medication management, and increased risk of chronic conditions. Tailoring care to the needs of older adults means considering not only their specific health issues but also the social and emotional aspects that come with aging.
Children represent another unique group requiring special attention. Pediatric care in an ambulatory setting calls for a nuanced understanding of developmental stages, family dynamics, communication strategies, and age-specific interventions. The provision of healthcare to children must encompass not only their physical well-being but also their emotional and developmental needs.
Pregnant women, too, have particular needs that must be addressed in an ambulatory care context. From prenatal screenings and check-ups to education on nutrition, exercise, and childbirth preparation, care must be multifaceted and attentive to both the mother and the developing fetus. The healthcare provider’s role includes not only medical care but also support and guidance throughout the pregnancy journey.
Individuals with disabilities present diverse challenges and opportunities in ambulatory care. Disabilities can range widely in nature and severity, and the care provided must be adapted to each person’s unique needs and abilities. This might include accessible facilities, adaptive equipment , individualized therapy, or other accommodations that empower individuals to lead fulfilling lives.
Put it into Practice
Sarah, a 72-year-old woman with mobility challenges and early signs of dementia, visits an ambulatory care clinic for a regular check-up. Her daughter, Emily, accompanies her and shares concerns about Sarah’s increased forgetfulness and difficulties in daily activities. The nurse conducts a comprehensive assessment, considering Sarah’s age, chronic conditions, cognitive decline, and Emily’s observations.
Recognizing the complexity of Sarah’s needs, the nurse collaborates with the healthcare team to create a tailored care plan. This plan includes adaptive equipment for mobility, medication management to address her chronic conditions, and a community-based support group for dementia. The nurse also involves Emily, providing her with resources and training to support her mother at home.
Reflective Items
- Comprehensive Assessment: How did the nurse’s comprehensive assessment of Sarah’s physical health, cognitive abilities, family dynamics, and chronic conditions influence the care plan? What additional information might be necessary for a more complete understanding?
- Tailored Care Plans: What elements in the tailored care plan specifically address Sarah’s unique needs as an elderly individual with mobility challenges and early signs of dementia? How do these elements demonstrate a patient-centered approach?
- Family and Community Involvement: How did the nurse involve Emily in the care process? What community resources were leveraged, and why were they considered important for Sarah’s care? How could the nurse continue to engage the family and community in Sarah’s ongoing care?
- Cultural Sensitivity (if applicable): Were there any cultural considerations that might impact Sarah’s care? If so, how were they addressed in the care plan, and what might be some potential challenges or opportunities related to these cultural factors?
- Ethical Considerations: What ethical considerations need to be taken into account when treating a patient like Sarah? How do patient rights and autonomy factor into the decisions made about her care?
Chronic disease patients require ongoing, often lifelong, management and support. The nature of chronic conditions means that care is not just about treating symptoms or managing a crisis but about a long-term, holistic approach to well-being. This includes monitoring, medication management, lifestyle adjustments, and regular check-ins, all tailored to the individual’s specific condition and needs.
Cultural considerations play an essential role in identifying and treating special populations. Healthcare providers must be aware of and sensitive to cultural beliefs, practices, and values that might impact the patient’s care experience. This includes language barriers, health beliefs, family dynamics, and more. A culturally sensitive approach ensures that care is respectful, appropriate, and effective for each individual, regardless of their cultural background.
The identification of these special populations is not merely a matter of categorization. It’s about recognizing the inherent complexity and diversity of human experience and needs and adapting care to be as inclusive, compassionate, and effective as possible. Whether dealing with age, developmental stage, physical ability, health condition, or cultural background, ambulatory care providers must be equipped with the understanding and tools necessary to provide the best possible care for all patients.
13.2 Assessment and Care Strategies
In the field of ambulatory care, especially when dealing with special populations, the process of care extends beyond mere diagnosis and treatment. It begins with a comprehensive assessment, a thorough and detailed evaluation of the patient’s health that considers not only the physical symptoms but also the mental, emotional, and social aspects. For special populations, this can mean delving deeper into specific challenges related to age, disability, chronic conditions, cultural background, or other factors unique to each patient. A comprehensive assessment isn’t just a snapshot of the current health status; it’s a foundational understanding upon which all subsequent care is built.
Building on the insights gained through this assessment, tailored care plans can then be developed. Unlike generic treatment protocols, tailored care plans are individually crafted to suit the particular needs, preferences, and characteristics of each patient. This individualized approach ensures that the care provided is not only medically appropriate but also aligned with the patient’s life goals, values, and daily realities. For an elderly patient, this might mean considering mobility challenges; for a child, it might include developmental milestones; for a chronic disease patient, it could involve ongoing management strategies.
However, the care of special populations in an ambulatory setting doesn’t stop at the individual level. It also involves family and community involvement. Families often play a crucial role in the daily care and well-being of special populations, and their insights, support, and collaboration can be invaluable in creating and implementing effective care plans. Community involvement can extend this support network even further, tapping into local resources, organizations, and cultural norms to create a holistic care environment that transcends the clinical setting.
Whether engaging with family members to understand a child’s behavior at home or working with community groups to support a disabled individual’s integration into local activities, this broader perspective adds depth and richness to the care process. It’s about seeing the patient not just as a set of symptoms or a clinical challenge but as a whole person, embedded in a network of relationships and communities.
Together, the comprehensive assessment, tailored care plans, and family and community involvement form a cohesive and holistic approach to care for special populations in ambulatory settings. It’s an approach that recognizes the inherent complexity and individuality of each patient and seeks to provide care that is not only medically sound but also humanly compassionate, culturally sensitive, and life-enhancing. It’s about moving beyond one-size-fits-all solutions to embrace the nuanced, multifaceted nature of healthcare, where every patient is seen, understood, and cared for in all their unique humanity.
13.3 Legal and Ethical Considerations
In the complex landscape of ambulatory care for special populations, legal and ethical considerations play a pivotal role, intertwining with almost every aspect of patient care.
Patient rights stand at the core of legal and ethical practice in healthcare. These rights encompass a range of entitlements and protections that empower patients to take an active role in their care, make informed decisions, and maintain dignity and autonomy. In the context of special populations, these rights may require extra attention, as certain groups may face challenges in understanding, communicating, or exercising their rights. For instance, elderly patients with cognitive impairments or children may need additional support to ensure that their rights are respected, understood, and upheld.
Coupled with respect for patient rights is the equally vital principle of confidentiality. Healthcare providers are legally and ethically bound to protect the privacy of their patients, ensuring that personal and medical information is handled with the utmost discretion. This confidentiality extends to all stages of care, from the initial assessment to ongoing treatment and communication with other healthcare professionals or family members. The balance of sharing necessary information for effective care while maintaining privacy requires careful consideration and often tailored strategies, particularly when dealing with vulnerable or complex cases within special populations.
Cultural sensitivity adds another layer to these legal and ethical considerations. As healthcare increasingly recognizes the diversity of patients, acknowledging and respecting cultural beliefs, practices, and values becomes essential. Whether it’s understanding traditional health beliefs, accommodating religious dietary restrictions, or communicating in a patient’s native language, cultural sensitivity ensures that care is not just legally compliant but also morally responsible and patient-centered. It’s about seeing the patient as a whole person, embedded in a cultural context, and adapting care to be as respectful and effective as possible.
Together, these three considerations form a triad of legal and ethical imperatives that guide the provision of ambulatory care for special populations. Patient rights, confidentiality, and cultural sensitivity are not isolated concepts but interconnected principles that influence and reflect each other. They shape the way healthcare providers interact with patients, design care plans, make decisions, and engage with families and communities. These principles don’t just ensure legal compliance; they also contribute to a higher standard of care, fostering trust, empathy, and excellence in a field where humanity, ethics, and the law must walk hand in hand.
13.4 Technological Interventions
Mobile health application for diabetes management in elderly patients.
One notable example of a mobile health application designed for a special population is a diabetes management app tailored for elderly patients. Managing diabetes requires careful monitoring of blood glucose levels, diet, exercise, and medication. For elderly individuals, especially those with cognitive impairments or limited technological skills, this management can be particularly challenging.
The specialized diabetes management app simplifies this process by incorporating large, easy-to-read fonts, intuitive navigation, voice commands, and personalized reminders. It allows users to log their blood glucose readings, meals, physical activity, and medication schedules in a user-friendly interface.
What sets this app apart for the special population of elderly patients is its integration with healthcare providers. Physicians and caregivers can access the patient’s data, allowing for real-time monitoring and timely interventions if something seems amiss. Additionally, the app offers educational videos and support tailored to the cognitive and sensory needs of older individuals, making it a holistic tool for empowerment and self-management.
This example illustrates how a mobile health application can be thoughtfully designed to meet the unique needs of a special population. By considering the specific challenges and requirements of elderly diabetes patients, the app becomes not just a technological tool but a bridge to better health, more engaged patients, and more coordinated care. It’s a testament to how technology, when adapted and applied thoughtfully, can create meaningful impacts in the lives of special populations.
In the rapidly evolving field of healthcare, technology plays a crucial role, and its applications are particularly resonant when it comes to special populations in ambulatory care. Two critical areas where technology has made significant strides are telemedicine and adaptive equipment.
Telemedicine represents a profound shift in how care is delivered, especially to special populations. Whether it’s a rural patient with limited access to specialized care or an elderly individual who struggles with transportation, telemedicine provides a bridge to quality healthcare right in their homes. Through video conferencing, remote monitoring, and online consultations, patients can connect with healthcare providers without the need for physical visits. This convenience can lead to more consistent care, timely interventions, and a more personalized relationship between patient and provider. The benefits of telemedicine extend beyond accessibility, too, enabling more flexible scheduling, reducing travel-related costs, and often leading to more engaged and empowered patients.
Adaptive equipment , on the other hand, focuses on enhancing the functionality and independence of individuals with disabilities or other specific needs. These tools and devices can range from simple modifications, like ergonomic handles on utensils, to sophisticated technologies such as voice-activated wheelchairs or computer software that assists with communication. The goal of adaptive equipment is to tailor the environment to the individual, rather than forcing the individual to adapt to an environment that may be inhospitable or even hostile to their needs. In the context of ambulatory care, adaptive equipment can significantly enhance the quality of life, improve therapeutic outcomes, and foster a sense of autonomy and dignity. It’s a technology that isn’t just about gadgets and innovation but about human values and well-being.
Both telemedicine and adaptive equipment reflect a broader trend in healthcare technology: the shift from a one-size-fits-all model to a more personalized, patient-centered approach. They showcase how technology can be harnessed not just to make care more efficient or advanced but to make it more humane, inclusive, and responsive to the unique needs of special populations. These technological interventions provide tools to overcome barriers, bridge gaps, and create opportunities, allowing healthcare providers to reach beyond the limitations of traditional care and engage with patients in ways that are meaningful, respectful, and transformative. It’s a marriage of innovation and empathy, where technology serves as an extension of the care provider’s skills and the patient’s potential, reshaping the very landscape of ambulatory care for special populations.
Challenges and Solutions
The provision of effective care for special populations in the ambulatory setting is not without its challenges. These challenges often extend beyond the immediate clinical context and involve complex issues related to navigating resources, communication, and collaboration with other healthcare providers. Let’s explore these challenges and the innovative solutions that have emerged to address them:
Navigating Resources: For patients and healthcare providers alike, the landscape of available resources can be confusing and difficult to navigate. Special populations often require specialized services, equipment, support, or funding, each of which may come from different sources, have unique eligibility criteria, and involve complicated application processes. The challenge here is not just identifying what resources are needed, but also how to access them efficiently and effectively. Solutions to this challenge often involve a combination of patient education, dedicated support staff such as social workers or case managers, and integrated technology platforms that can streamline and simplify the resource navigation process. By providing clear pathways, guidance, and support, these solutions empower patients and providers to access the resources they need without getting lost in a maze of bureaucracy.
Communication: Effective communication is a cornerstone of healthcare, but it can be especially challenging in the context of special populations. Whether it’s language barriers, cognitive impairments, cultural differences, or simply the complexity of care, communication issues can lead to misunderstandings, missed opportunities, and suboptimal care. Solutions to these challenges often hinge on tailored communication strategies that recognize and address the unique needs and characteristics of each patient. This might include the use of interpreters, specialized communication tools, cultural competence training, or a more conscious effort to engage patients and families in clear, open dialogue. By recognizing that communication is not a one-way street but a dynamic and nuanced process, these solutions foster a more collaborative, empathetic, and effective care relationship.
13.5 Collaboration with Other Healthcare Providers
The multifaceted nature of care for special populations often requires collaboration across various healthcare providers, from primary care physicians to specialists, therapists, social workers, and more. This collaboration can be complex, as it involves coordinating care across different settings, disciplines, and systems. Challenges may arise due to conflicting treatment plans, lack of information sharing, or simply the logistical difficulties of scheduling and coordination. Solutions to these challenges often involve integrated care models, shared electronic health records, regular multidisciplinary team meetings, and clearly defined roles and responsibilities. By fostering a culture of collaboration, transparency, and shared purpose, these solutions ensure that the care provided is not fragmented or contradictory but unified, coherent, and patient-centered.
Together, these challenges and solutions paint a picture of a field that is both complex and innovative. They highlight the intricacies of providing care to special populations in an ambulatory setting, where the medical, social, cultural, and systemic dimensions intersect and interact. They also showcase the creativity, resilience, and dedication of healthcare providers who continually strive to overcome these challenges, finding new ways to enhance care, build relationships, and create a healthcare experience that is truly responsive to the unique needs and potentials of each patient. It’s a dynamic and inspiring landscape, where challenges are not just obstacles but opportunities for growth, learning, and transformation.
Chapter 13 Summary
This chapter explored the multifaceted and intricate field of special populations in ambulatory care. We began by identifying what constitutes special populations, including the elderly, children, pregnant women, individuals with disabilities, chronic disease patients, and cultural considerations. Assessment and care strategies were then elaborated, focusing on comprehensive assessments, tailored care plans, and the importance of family and community involvement.
Legal and ethical considerations such as patient rights, confidentiality, and cultural sensitivity were addressed, highlighting their interconnectivity and influence on patient care. Technological interventions like telemedicine and adaptive equipment were explored, illustrating how they have revolutionized care delivery for special populations.
We then delved into challenges and solutions in navigating resources, communication, and collaboration with other healthcare providers, providing insights into the complexities and innovative strategies to overcome these challenges. The chapter paints a vivid picture of the dynamic, responsive, and empathetic landscape of ambulatory care for special populations, emphasizing both the challenges and the opportunities that lie therein.
Key Takeaways
- Special populations in ambulatory care include diverse groups such as the elderly, children, pregnant women, individuals with disabilities, and chronic disease patients, requiring specific considerations.
- Comprehensive assessment of individual needs is crucial for creating effective and tailored care plans.
- Family and community involvement are vital components in creating a holistic care environment that supports the unique needs of the patient.
- Upholding patient rights, ensuring confidentiality, and practicing cultural sensitivity are fundamental legal and ethical obligations in healthcare.
- The integration of telemedicine and adaptive equipment is transforming healthcare delivery, making it more accessible and personalized for special populations.
- Navigating the complex landscape of healthcare resources requires understanding and guidance to ensure that necessary services and support are accessible.
- Clear and effective communication strategies must be implemented to foster understanding and cooperation between healthcare providers and patients.
- Collaboration with other healthcare providers is essential for ensuring a cohesive, unified approach to care that meets all aspects of a patient’s needs.
- Addressing the challenges of care for special populations requires innovative solutions that focus on individualized care, resource navigation, and interdisciplinary collaboration.
- Mobile health applications, tailored to specific needs such as elderly diabetes management, can provide essential support and empowerment for special populations.
Check Your Understanding
Now that you have completed this chapter, take a moment to review what you’ve learned and assess your understanding. Please answer the following 10 items designed to reinforce key concepts from this chapter. You can navigate through the questions by clicking the blue right-facing arrow located at the bottom right of the question block. This exercise will help ensure that you have grasped the essential information before moving on. Your responses can provide valuable feedback on areas where you may need further review or where you have a strong understanding of the material.
Groups of individuals who require specific attention, tailored approaches, and specialized care plans within a healthcare setting, such as the elderly, children, pregnant women, individuals with disabilities, and chronic disease patients.
Tools and devices modified or specially designed to assist individuals with disabilities or other special needs. These play a vital role in enhancing the independence and quality of life for special populations in ambulatory care
The awareness, understanding, and respect of cultural differences, including beliefs, practices, and values, in healthcare provision. This concept is crucial in the treatment of diverse special populations to ensure equitable and respectful care.
The use of technology to provide clinical health care from a distance, often used to enhance the accessibility and efficiency of care for special populations.
Foundations of Ambulatory Care Nursing Copyright © by Stacey Hobbick is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book

IMAGES
COMMENTS
Feb 20, 2023 · The elderly population (age >65 years) is increasing throughout the world, leading to increased hospitalization. There was a 16.7% increase in elderly hospitalization from 2003-2009 in the United States. This rising hospitalization has impacted healthcare services delivery.[1] With the aging population comes a multitude of chronic conditions. It is estimated that 9 out of 10 Americans have at ...
E. See Box 5-2 for a comprehensive nursing assessment tool written by the authors of this chapter, titled Special Populations Needs Assessment Tool, that can be used to obtain information from the client about his or her special needs in order to plan care. This tool can be adapted, based on the individual being cared for.
1) _____Assess the effect of a patient’s disability on his/her ability to obtain health care. (Assessment should address the interaction of person’s disability and health care, his or her ability to manage self-care activities, follow health care recommendations, and obtain preventive health screening and follow-up care.)
Feb 20, 2023 · The elderly population varies in cognitive, physical, and social functioning and thus requires different levels of care based on individual needs and functional status. Geriatric assessment, thus, includes a coordinated approach for the physical, functional, and psychosocial assessment of the elderly and formulate an integrated plan of care.
Examples of special populations include obstetric examination during pregnancy, labor and delivery, and the postpartum period, newborn assessment, pediatric assessment, and geriatric assessment. This chapter will demonstrate how the health assessment is adapted for the pediatric and geriatric populations.
Examples of such include pediatric assessment, geriatric assessment, newborn assessment and obstetric examination during pregnancy, labor and delivery and the postpartum period. There is a wide diversity of special populations but this chapter will provide information on pediatric assessment and geriatric assessment, wherein nurses will highly ...
The Adult Needs and Strengths Assessment (ANSA) is a multi-purpose tool developed for adult’s behavioral health services to support decision making, including level of care and service planning, to facilitate quality improvement initiatives, and to allow for the monitoring of outcomes of services.
The model of care is the structure of the care management processes and systems to provide coordinated and appropriate care for our special needs members. The key model of care objectives specific to the unique needs of the SNP population are to: •Evaluate and improve members’ access to clinical and administrative services.
Define and identify special populations in the context of ambulatory care. Recognize the unique needs and challenges of special populations. Apply comprehensive assessment techniques tailored to each special population. Describe the legal and ethical considerations in treating special populations.
Jan 1, 2021 · Falls are the leading cause of injury among adults aged ≥65 years (older adults) in the United States. In 2018, an estimated 3 million emergency department visits, more than 950,000 ...